20 Common Examples of Ethical Dilemmas in Nursing + How to Deal With Them

If you are a nurse, chances are you have faced situations where you had to make decisions based on your belief of whether something is right or wrong, safe or unsafe. This type of decision is based upon a system of ethical behavior. It is essential that all nurses develop and implement ethical values into nursing practice. If this sounds familiar, you may be asking, "What are the common examples of ethical dilemmas in nursing?" There are many things that could be considered an ethical dilemma in nursing, and it is important for nurses to know how to address them when they occur. In this article, I will share the 20 most common examples of ethical dilemmas in nursing and offer some insight into handling them.

What is an Ethical Dilemma in Nursing?
5 main reasons why nurses face with ethical dilemmas in nursing.
1. Patients or their loved ones must make life or death decisions 2. The patient refuses treatment 3. Nursing assignments may contradict cultural or religious beliefs 4. Nursing peers demonstrate incompetence 5. Inadequate staffing
How to Identify Ethical Dilemmas in Nursing?
What are the common examples of ethical dilemmas in nursing, example #1: pro-life vs. pro-choice, ethical dilemma:, how to deal with this ethical dilemma:, example #2: protecting the adolescent’s right to privacy, example #3: empirical knowledge vs. religious beliefs, example #4: parent refuses to vaccinate child, example #5: personal and professional boundaries related to social media, example #6: nurse is instructed to have patient with low literacy level to sign consent for treatment, example #7: end-of-life decision-making, example #8: inadequate resources to provide care, example #9: former patients - to date or not to date, example #10: informed consent, example #11: inadequate staffing, example #12: spirituality vs. science, example #13: patient addicted to prescription pain medication, example #14: duty and compassion do not align with facility safety protocols, example #15: patient does not have an advanced directive, example #16: incompetence among nursing peers, example #17: disclosing the seriousness of medical conditions, example #18: questioning physician orders, example #19: asked to work in a department without training, example #20: beneficence vs. autonomy, 4 consequences of avoiding ethical dilemmas in nursing, 1. nurses can quickly experience burnout., 2. avoiding ethical dilemmas in nursing can lead to legal issues., 3. nurses who avoid ethical dilemmas could lose their jobs., 4. loss of licensure:, my final thoughts.

10 Examples of Ethical Dilemmas in Nursing

When caring for human lives, the decisions you have to make as a nurse are anything but black and white. In addition to taking vital signs and doing dressing changes, there are a realm of tough choices and ethical dilemmas that nurses have to face every day.
Picture this: a nurse finds himself torn between respecting a patient's right to refuse treatment and their deteriorating health. Moral puzzles like these leave even the most experienced nurses scratching their heads and feeling caught between a rock and a hard place. However, understanding how to handle ethical dilemmas isn't just a theoretical exercise. It's a crucial skill that nurses need to have in their toolkits.
The nursing code of ethics acts as a guide for nurses to help in these decisions, but it can be helpful to see actual examples of ethical dilemmas in nursing and what a nurse should do with each of them. That’s exactly what this article is about.
Find Nursing Programs
Nurses helping nurses: why you can trust nurse.org.
As the leading educational website for nurses by nurses, Nurse.org is committed to editorial integrity and data-driven analysis.
✔ Content written by 80+ licensed, practicing nurses who are experts in their respective specialties. Learn more about our nurse contributors .
✔ Transparent, trusted data sources from the U.S. Bureau of Labor and Statistics (BLS), Payscale, ZipRecruiter and Glassdoor. Learn more about our data resources .
✔ Consistent article updates to ensure they are as relevant and accurate as possible, utilizing the latest data and information when it becomes available.
10 Common Ethical Dilemmas in Nursing
While there are many different situations in which a nurse may find themselves dealing with an ethical dilemma, here are 10 common ethical dilemmas in nursing to consider and how a nurse might deal with them:
1. Patient Autonomy vs. Beneficence
Balancing a patient's right to make decisions about their own care with the nurse's duty to promote their overall well-being.
Let's say a patient diagnosed with diabetes refuses to take insulin, despite it being essential for controlling their blood sugar levels and preventing serious complications.
In dealing with this situation, a nurse should follow the nursing code of ethics and take the following steps:
Respect Autonomy: Respect the patient's right to make decisions about their own care, even if they disagree with those decisions.
Provide Information: Ensure the patient has accurate and comprehensive information about the treatment, including its benefits, risks, and alternatives. This allows the patient to make an informed decision.
Assess Understanding: Engage the patient in open and non-judgmental communication to assess their understanding of the treatment and the potential consequences of refusing it.
Collaborative Decision-Making: Engage the patient in collaborative decision-making. Involve them in discussions and explore alternatives that align with their values and preferences. This approach fosters a sense of working together and mutual respect.
Seek Additional Perspectives: If the patient's decision still conflicts with the nurse's professional judgment and poses a significant risk to the patient's health, the nurse should seek guidance from the healthcare team and the nurse manager or supervisor they report to.
Document the Process: Throughout the decision-making process, carefully document all discussions, assessments, and the patient's decisions. This documentation serves as evidence that the nurse has fulfilled their ethical and professional responsibilities.
>> Related: What is Autonomy in Nursing?
2. Confidentiality vs. Duty to Warn
Struggling with maintaining patient confidentiality while also considering the potential harm to others if vital information is not shared.
Imagine a scenario where a nurse working in a mental health facility becomes aware that a patient with a history of violent behavior has confided in the nurse about their plan to cause harm to their former partner.
The nurse finds themselves in a challenging ethical dilemma: on one hand, they have a duty to maintain the confidentiality of the patient's personal information, and on the other hand, they have an obligation to protect other people from harm.
To deal with this situation, the nurse should take the following steps:
Evaluate the Severity of the Threat: Carefully assess the level of risk involved in the patient's intentions. Is there an immediate and credible threat to the safety of the potential victim? Consider factors such as the patient's history, current mental state, and access to means for carrying out the harm.
Engage in a Therapeutic Relationship: Explore the underlying issues and reasons behind the patient's harmful intentions. Attempt to address any underlying issues or triggers that may contribute to their behavior and encourage them to seek alternative ways to cope.
Seek Supervision and Consultation: It’s important for the nurse to consult with their supervisor or team members about the appropriate course of action to ensure the safety of the potential victim.
Follow Legal and Ethical Guidelines: Be aware of local laws and regulations regarding the duty to warn or protect. If there is a legal obligation to disclose information in order to prevent harm, the nurse should adhere to those requirements while minimizing the breach of confidentiality to the extent possible.
Document the Process: Document all steps taken, including the patient's disclosure, assessments, consultations, and decisions made. This documentation serves as evidence that the nurse acted ethically, responsibly, and in line with professional standards.
3. End-of-Life Care
Managing the ethical complexities around decisions about withdrawing or withholding life-sustaining treatment, considering the patient's wishes, quality of life, and family dynamics.
For example, consider the situation where a nurse is caring for an elderly patient with a terminal illness. The patient expresses the desire to die a peaceful death without aggressive interventions. However, the patient’s family opposes this and wants “everything medically possible” to be done to save the patient’s life.
The nurse finds themselves in a complex ethical dilemma, torn between honoring the patient's wishes and respecting the concerns of the family.
Here’s how the nurse might address this situation:
Communication and Education: Engage in open and compassionate communication with both the patient and the family about the patient's medical condition. Discuss the patient’s prognosis, available treatment options, and the potential benefits and downsides of continuing or discontinuing life-sustaining measures.
Respect for Autonomy: Advocate for the patient's right to self-determination and respect their wishes regarding end-of-life care.
Collaboration and Mediation: Facilitate a respectful and open dialogue, promoting a collaborative decision-making process. The nurse can involve the healthcare team, including palliative care specialists and social workers, to provide support, guidance, and mediation to resolve this situation.
Consider Ethical Decision-Making Frameworks: The nurse should use ethical principles in the nursing code of ethics, such as beneficence, non-maleficence, autonomy, and justice, to analyze the situation and guide their actions. By considering the patient's values, goals, and potential impact on their quality of life, the nurse can advocate for the most ethically appropriate course of action.
Supportive Care: Regardless of the final decision made, the nurse should provide holistic and supportive care to the patient and their family. This includes addressing physical, emotional, and spiritual needs, ensuring optimal comfort, and facilitating open communication to foster a sense of trust and understanding.
4. Resource Allocation
Facing the difficult task of distributing limited resources fairly and ethically among patients, especially during times of scarcity or emergencies.
Consider this scenario: During a severe flu outbreak, a nurse working in a hospital emergency department faces the ethical dilemma of resource allocation. The hospital is overwhelmed with patients and the available resources, such as beds, ventilators, and medications are limited. The nurse must make decisions about which patients receive the resources, balancing the needs of the patients in their care while also considering the needs of other patients in the hospital.
The nurse should manage this situation with fairness and transparency, using the following steps:
Prioritization and Triage: Follow established guidelines and protocols for triaging patients based on the severity of their condition and their likelihood of benefiting from the available resources. This ensures that decisions are made based on clinical needs rather than personal biases.
Open Communication: Maintain open and transparent communication with patients and their families. Explain the challenges faced due to limited resources and the criteria being used for resource allocation. This promotes understanding and trust, even in difficult circumstances.
Collaboration and Consultation: Work collaboratively with the healthcare team, including physicians and hospital administrators, to make informed decisions about resource allocation. Seeking input from multiple perspectives helps ensure fairness and accountability.
Consider Ethical Decision-Making Frameworks: Use the ethical principles of fairness and justice in the nursing code of ethics to guide the nurse’s actions. By considering factors like the potential benefits, risks, and overall impact on patients and the community, the nurse can strive to allocate resources in an equitable and ethical manner.
Advocacy and Support: Advocate for the well-being and rights of their patients, even when difficult decisions must be made.
5. Informed Consent
Ensuring patients have a clear understanding of the risks, benefits, and alternatives of proposed treatments or procedures before they provide consent.
Here’s an example of how this ethical dilemma could occur: A nurse assists a physician who is rushing to obtain informed consent for a surgical procedure, despite the patient's pain and anxiety. However, the nurse quickly recognizes the patient's limited understanding of the procedure’s implications, raising ethical dilemmas regarding informed consent.
To handle this situation, the nurse should follow these steps:
Ensure Adequate Information: Intervene respectfully but assertively and ask the physician to slow down and provide the patient with complete information about the procedure, risks, benefits, potential outcomes, and available alternatives.
Clarify Patient Understanding: Speak with the patient and assess their understanding of the information provided. Encourage the patient to ask questions and address any concerns they may have.
Advocate for Time and Support: If the patient appears overwhelmed or is struggling to comprehend the information, the nurse should advocate for additional time or resources, such as involving a family member or providing educational materials or an interpreter (if appropriate) to support the patient in making an informed decision.
Document the Process: Document the steps taken to address the concerns related to informed consent. Be sure to include any discussions, explanations provided, patients' questions, and their ultimate decision. Accurate documentation demonstrates the nurse's commitment to upholding ethical standards and professional accountability.
6. Cultural and Religious Beliefs
Navigating conflicts between a patient's cultural or religious values and the standard practices or protocols of healthcare.
In a multicultural society, nurses often encounter ethical dilemmas when a patient's cultural or religious beliefs clash with the standard practices or protocols of healthcare. An example is when a nurse is caring for a patient from a cultural background who strongly believes in traditional healing methods and is hesitant to accept Western medicine.
In this situation, the nurse should have a culturally sensitive discussion with the patient and demonstrate respect for diversity. Here are the steps the nurse should take:
Culturally Competent Assessment: Conduct a culturally competent assessment to understand the patient's cultural and religious beliefs, values, and preferences regarding healthcare. This requires active listening, open-mindedness, and avoiding assumptions or stereotypes.
Establish Trust and Rapport: Build a trusting relationship with the patient by acknowledging and respecting their cultural and religious beliefs. This can be achieved through effective communication, empathy, and demonstrating cultural humility.
Collaborative Decision-Making: Engage the patient and their family in collaborative decision-making regarding their healthcare. Respectfully discuss the patient's beliefs and preferences, and explore opportunities to integrate traditional healing practices with evidence-based Western medicine.
Consultation and Education: If there are concerns about the patient's well-being or the appropriateness of certain traditional healing methods, the nurse should seek guidance from a cultural consultant, interpreter, or healthcare team.
Advocacy and Liaison: Serve as an advocate for the patient, ensuring their cultural and religious rights are respected within the healthcare system. This may involve facilitating communication between the patient and healthcare providers, ensuring the provision of culturally competent care, and addressing any cultural or religious barriers that may arise.
7. Impaired Colleague
Grappling with the ethical responsibility of reporting concerns about a colleague's impairment due to substance abuse or mental health issues.
This situation might occur when a nurse becomes aware that a nursing colleague is impaired while on duty. The impaired nurse exhibits erratic behavior and smells strongly of alcohol. The nurse who witnesses this behavior finds themselves in a challenging ethical dilemma, torn between their duty to ensure patient safety and their loyalty to their colleague.
Nevertheless, the nurse needs to prioritize patient safety and act professionally by following these steps:
Immediate Concern for Patient Safety: The nurse's primary responsibility is to ensure the safety and well-being of patients. If they observe signs of impairment in their colleague that could compromise patient safety, they should take immediate action.
Reporting: The nurse should report their observations and concerns to the appropriate authority within the healthcare facility, such as the nurse manager or supervisor. This report should be made objectively without personal judgments or assumptions and with a focus on patient safety.
Confidentiality and Professionalism: Maintain confidentiality throughout the reporting process, being mindful not to disclose personal details of the impaired colleague unless necessary for the investigation.
Collaboration and Support: Collaborate with the healthcare team and support the impaired colleague's well-being by encouraging them to seek appropriate help and support, such as employee assistance programs or counseling services.
Ethical Obligation: Nurses have an ethical obligation to protect the welfare of patients and maintain the standards of the nursing profession. This includes recognizing and addressing impairment issues among colleagues to ensure safe and quality care.
8. Professional Boundaries
Striking a balance between providing compassionate care and maintaining appropriate professional boundaries, particularly when it comes to personal relationships with patients.
In this example, let’s look at a scenario where a nurse develops a close friendship with a patient and begins sharing too many personal details about their own life unrelated to the patient’s healthcare needs.
When the nurse realizes what’s happening, they need to prioritize maintaining professional boundaries and act in the best interest of the patient by following these steps:
Recognize the Boundary Issue: Use personal reflection to recognize when professional boundaries are being crossed or compromised. Acknowledging this ethical dilemma is the first step toward resolving it.
Reflect on the Nurse-Patient Relationship: The nurse should remind themselves of their professional role, the duty of care, and the need to maintain objectivity and professional distance.
Reestablish Boundaries: Take appropriate actions to reestablish and reinforce professional boundaries with the patient. This may involve redirecting conversations back to the patient's healthcare needs, avoiding personal disclosures, and focusing on the patient's well-being.
Seek Guidance and Supervision: If the situation becomes challenging to resolve alone, the nurse should seek help from a supervisor, nurse manager, or experienced nursing team member. Consulting with experienced professionals can provide valuable insights and support in addressing this ethical dilemma.
Continuous Professional Development: Engage in ongoing professional development and education regarding nursing ethics and setting professional boundaries. Staying current on ethical guidelines and participating in discussions and training on maintaining professional boundaries can help prevent future boundary issues with patients.
9. Whistleblowing
Facing the ethical dilemma of reporting concerns about wrongdoing or unethical practices within the healthcare system, despite potential professional and personal repercussions.
An example of whistleblowing would be when a nurse becomes aware that a colleague is stealing controlled substances from the medication supply. The nurse decides to report this to their supervisor because it compromises patient safety and violates professional and legal standards. However, the nurse is worried about their colleague being disciplined and possibly losing their license.
Here are the steps the nurse should follow:
Gather Evidence: Collect factual evidence such as documentation discrepancies in medication records, witnessing the colleague's actions, or capturing any other supporting documentation.
Consult with Colleagues: Seek advice from trusted colleagues, supervisors, or mentors within the healthcare organization. Discuss the situation and determine the best course of action. It’s important to maintain confidentiality during these discussions to protect both the patient and the nurse making the report.
Follow the Proper Chain of Command: Follow the established reporting channels within their healthcare organization. This typically involves reporting concerns to a supervisor, nurse manager, or a designated ethics or compliance hotline. Ensure that the report is made in writing and contains all relevant details and evidence.
Protection and Confidentiality: Be familiar with the whistleblower protection policies and laws in their jurisdiction. The nurse should ensure that their report is treated confidentially and that appropriate steps are taken to protect them from retaliation.
Documentation: Keep a detailed record of all actions taken, including the date and time of the incident, any conversations or consultations, and copies of the report submitted. This documentation helps demonstrate the nurse's commitment to reporting and acting in accordance with professional and ethical standards.
10. Ethical Use of Technology
Considering the ethical implications of using technology in healthcare, such as maintaining patient privacy and security, avoiding biases in algorithms, and ensuring equitable access to care.
An example of this ethical dilemma could occur when a nurse becomes concerned about potential biases in an algorithm and decides to report this to her supervisor. She recognizes that an algorithm where she works may disproportionately allocate resources based on patient factors such as age, race, and gender, resulting in inequitable access to care.
The nurse should advocate for equitable care by taking these steps:
Investigate and Evaluate: Become familiar with the AI algorithm being used and investigate its development process. Assess whether the algorithm has been validated and tested for biases and fairness.
Raise Concerns: If the nurse identifies biases or inequities in the algorithm, they should communicate their concerns to the appropriate individuals, such as nurse leaders, healthcare administrators, or the technology implementation team.
Collaborate for Improvement: Engage in collaborative discussions with the healthcare team, including the nursing supervisor, IT specialists, and data scientists. Work with the team to develop strategies to eliminate biases and ensure equitable use of the technology for all patients.
Promote Patient Advocacy: Advocate for the rights and well-being of the patients who may be affected by the technology. This involves ensuring informed consent and transparency regarding the use of AI algorithms. Patients should have the opportunity to understand and discuss the potential biases and their impact on their care.
Continuous Evaluation: Advocate for ongoing evaluation and monitoring of all AI technology being used in patient care to identify and resolve biases or unintended consequences.
Ethical dilemmas are common in nursing and can be difficult to deal with. But you don’t have to make the decisions about these issues alone. Seek out the support and input of your nursing colleagues, supervisor, or nurse manager. By doing so, you will feel more comfortable and confident about how to handle the ethical dilemma you find yourself in.
*This website is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease.

Leona Werezak BSN, MN, RN is the Director of Business Development at NCLEX Education. She began her nursing career in a small rural hospital in northern Canada where she worked as a new staff nurse doing everything from helping deliver babies to medevacing critically ill patients. Learning much from her patients and colleagues at the bedside for 15 years, she also taught in baccalaureate nursing programs for almost 20 years as a nursing adjunct faculty member (yes! Some of those years she did both!). As a freelance writer online, she writes content for nursing schools and colleges, healthcare and medical businesses, as well as various nursing sites.
BSN & MSN University of Saskatchewan
What can we help you find?
A systematic approach to ethical decision-making for nurses.

December 2022
This article, from the Nurses Service Organization, reviews a model that nurses can use to better understand conflicting issues and navigate ethical dilemmas.
Nurses are well aware of patients’ rights, such as the right of patients for self-determination (the right to make decisions about their own care). This right has even been codified in law as a result of the Patient Self-Determination Act (PSDA) of 1991, which requires healthcare agencies receiving Medicare and Medicaid reimbursement to provide information about advance directives. Patients’ rights, like self-determination, also play a role in ethics. For example, Provision 1.4 of the American Nurses Association (ANA) Code of Ethics for Nurses with Interpretive Statements ( the Code) states that the patient has a right to self-determination.
In the clinical setting, ethical conflicts related to self-determination and other ethical principles are not unusual. Consider these possible scenarios: A family member disagrees with an advance directive that a patient completed now that the patient is unable to speak for themself. A patient declined to receive a potentially life-saving treatment even after receiving information about the process. A nurse wonders if a patient has received enough information from the physician to truly give informed consent. How can these types of ethical dilemmas be resolved? Taking a systematic approach can help you navigate toward a decision, but first it is useful to understand how legal issues relate to ethical principles.
Legal responsibilities
Even though the Code relates to ethics and not the law, attorneys could turn to it for evidence that a nurse’s behavior did not meet the standard of care. For example, the Code states, “Nurses preserve, protect, and support those rights by assessing the patient’s understanding of the information presented and explaining the implications of all potential decisions.” If you fail to act when you think a patient did not receive enough information about a treatment decision, you could be held liable.
In addition, keep in mind that principles such as self-determination and patient autonomy applies not only to end-of-life care but to all treatment decisions. Therefore, going against a patient’s wishes could put you in legal jeopardy. For example, drawing blood from a patient who states he does not want lab work done could be considered battery.
To help avoid legal peril, use a systematic approach to making ethical decisions, based on ethical principles ( see Key ethics principles ). One such approach is a framework for ethical decision making from the American Counseling Association (ACA). While written for counselors, the framework outlines seven steps any healthcare professional can use to approach ethically ambiguous situations:
#1. Identify the problem.
To identify the problem, you first need to gather information related to the situation. Focus on facts, not assumptions. Consider whether the issue is related to yourself and what you are doing (or not doing) or is related to the patient or the patient’s loved one and what they are doing or not doing. For example, in the case of a young teenager who has not been informed he has brain cancer at the request of his parents, an ethical issue relates to the dynamics of the parents not wanting the diagnosis to be shared and the healthcare professionals who must consider the impact on the patient.
Be sure you are truly facing an ethical problem and not a clinical, legal, or professional one or a combination. Other considerations include whether the issue is related to technology (e.g., mechanical ventilation) or organizational policy. For example, legal statutes and organizational policy related to removing a patient from life support could conflict with what you see as the right ethical path. If there is any element of a legal issue involved, be sure to consult your organization’s risk management or legal department, or an attorney.
#2. Apply the code of ethics.
Once you have identified the problem, turn to the Code . In some cases, the answer may be there. For example, a patient gives you a computer tablet as a thank-you gift. You had wanted to purchase a new tablet to replace your old one, but you are unsure if you should accept the gift. Provision 2.4 of the Code states, “Accepting gifts from patients is generally not appropriate.” The provision goes on to state that one factor to consider is the value of the gift. The cost of a tablet means you should decline the gift. (In addition, your organization likely has a policy that prohibits gifts from patients.)
If the issue is not resolved by codes of ethics, you will need to move on to the next step.
#3. Determine the nature and dimensions of the dilemma.
To accomplish this task, analyze the dilemma in terms of ethical principles. Determine which principles apply and which have priority in this case. For instance, a patient with a history of chronic pain is asking for an early refill of his narcotic prescription. Granting the prescription might meet the principle of beneficence in the short term by providing pain relief but could violate the principle of nonmaleficence by putting the patient at risk of substance misuse.
As part of your analysis, consider consulting the literature to ensure current, evidence-based practice. Thinking and consulting with colleagues or managers can also help you see other points of view. Another excellent resource is your organization’s ethics committee. In certain situations, you may even want to consult with your state or national professional association for input.
#4. Generate potential courses of action.
This is the time for brainstorming ideas for actions to take. Write the ideas down without taking time to consider whether they are viable. Having another colleague help you with this step is a good idea.
#5. Consider the potential consequences of all options and determine a course of action.
Now you should evaluate the potential courses of action you identified. Consider each option in the context of the information you have and evaluate the positive and negative effects of the option in relation to ethical principles you have identified. You will also want to evaluate each action for the potential effects on you, the patient, and any others who will be affected, for example, the patient’s family or the organization. It may be helpful to write a list of pros and cons for each option.
Toss out options that are problematic and take a closer look at the remaining ones, ultimately picking the one that best fits the situation.
#6. Evaluate the selected course of action.
Once you have chosen a course of action, test it to determine if it truly is the best option. The three “tests” are justice, publicity, and universality:
- To apply the test of justice , consider your own sense of fairness and whether you would treat others the same in the situation.
- To apply the test for publicity , ask if you would want your behavior reported in the media.
- And to apply the test for universality , consider whether you would recommend the same course of action to another nurse.
If your option does not fulfill all three tests, return to the start of the process. You may find that you did not properly identify the problem. If your choice met the tests, you are ready to move forward.
#7. Implement the course of action.
Know that just because you feel the action is the right one does not mean it will be easy to carry out. You may need to engage in stress reduction techniques before and after the action.
Related Posts

Open to What is Possible

Federal Guidelines on OTP: An APNA expert weighs in

Youth Suicide Prevention Experts Identify Key Considerations for PMH Nurses
Your dynamic community of psychiatric-mental health nurses..
Connect with fellow psychiatric-mental health nurses, be the first to know about evidence-based resources and programs, and participate in exclusive opportunities to advance the care and treatment of those with mental health & substance use needs.
JOIN TODAY MEMBER COMMUNITY

- Work Environment
20 Most Common Ethical Dilemmas in Nursing & Solutions

As a nurse, you often find yourself in situations that require you to make tough decisions, balancing the best interests of your patients with ethical considerations. These ethical dilemmas can arise due to conflicting values, legal obligations, or scarce resources.
In this article, we will explore some common examples of ethical dilemmas in nursing, each accompanied by a real-life scenario that highlights the complexities faced by healthcare professionals. Let’s dive in.
Example #1: Balancing Patient Autonomy and Beneficence
Example #2: maintaining patient confidentiality vs ensuring public safety, example #3: disclosure of medical errors to patients, example #4: allocating limited resources during a pandemic, example #5: end-of-life decision-making, example #6: balancing patient confidentiality and duty to protect, example #7: cultural sensitivity and respect for diversity, example #8: conflict of interest in healthcare decision-making, example #9: informed consent and pediatric patients, example #10: boundaries and professional relationships, example #11: confidentiality and reporting child abuse, example #12: patient autonomy and end-of-life decision-making, example #13: balancing autonomy and well-being for a dementia patient, example #14: medication administration and patient refusal, example #15: resource allocation during a pandemic, example #16: cultural competence and end-of-life care, example #17: confidentiality and risk of harm, example #18: patient autonomy and non-adherence to treatment, example #19: informed consent and decision-making capacity, example #20: privacy and confidentiality in the age of electronic health records.
Scenario: Imagine you’re a hardworking nurse in a busy hospital. One day, you face an interesting challenge. You have a 75-year-old patient, Mrs. Johnson, who needs to undergo a surgical procedure due to her chronic heart condition. But during your talk about the operation, she shares her fears about possible complications and not waking up from anesthesia. She insists on not having the surgery even though it could save her life. As her nurse, you know how important it is to listen to your patient’s wishes but also want to do what’s best for their health.
Ethical Dilemma: This situation creates a serious ethical problem for you. On one hand, there’s the need to respect the patient’s choice in their healthcare decisions, called “patient autonomy.” Here it would mean acknowledging Mrs. Johnson’s concerns and respecting her decision not to have the surgery. However, on the other hand, there’s an equally important principle of doing good for your patient – that is “beneficence”. From this perspective, moving forward with the surgery could dramatically improve her quality of life and may be crucial for her survival.
This conflict between respecting a patient’s wishes and wanting to ensure their well-being can be tough for nurses like you. You’re expected to support your patients’ choices but also have a duty towards promoting their health. In Mrs.Johnson’s case, because she doesn’t want necessary surgery due to fear of complications, it becomes tricky for you and your team to balance these principles while providing top-notch care.
As part of your responsibility as a healthcare professional, it falls upon you to educate patients like Mrs.Johnson so they understand their situation fully and can make sound decisions about their own health care based on facts rather than fears alone.
Solution and Tips: Tackling ethical dilemmas in nursing calls for patience and careful thinking while keeping the principles of beneficence (doing good) at heart along with recognizing patient’s autonomy (their right). Here are some simple tips that will help:
- Open communication: Make sure all lines of communication with your patients are open; encourage them to share worries or doubts they might have.
- Patient education: Explain all options clearly; tell them what could happen if they choose each option.
- Joint decision-making: Include everyone – patients, families and medical teams – in deciding what steps should be taken next.
- Ethical guidelines: Keep revisiting principles like autonomy (patient independence), beneficence (doing good), non-maleficence (not causing harm) etc., as these provide guidance when faced with difficult situations.
- Consultation: If needed don’t hesitate consulting colleagues or ethics committee members who are knowledgeable in such matters; this can provide varied perspectives which might prove useful in resolving issues.
Scenario: Imagine you’re a nurse at a psychiatric facility. One day, Mr. Anderson, a patient dealing with severe mental illness, shares his violent thoughts towards someone outside the facility with you. As a nurse, you value patient confidentiality and their privacy. But, you also have an essential role in ensuring public safety and preventing harm.
Ethical Dilemma: This situation presents a challenging ethical dilemma – how to balance between protecting patient confidentiality and ensuring public safety? When you respect privacy in healthcare, patients trust you more. But Mr. Anderson’s violent intentions put the welfare of others at risk.
This ethical dilemma is about finding the right balance between maintaining patient confidentiality and fulfilling your duty to protect potential victims from harm. It’s not easy to navigate this boundary – protecting Mr. Anderson’s rights and well-being on one hand while also addressing the potential harm that might fall upon others on the other hand.
Keeping your patients’ information confidential helps develop trust and makes them feel safe when sharing sensitive information with you. But if there’s danger involved for people outside your healthcare setting, it creates a moral quandary for healthcare professionals like yourself.
Solution and Tips: Resolving such dilemmas involves careful thought process paired with abidance by legal and ethical guidelines:
- Check how serious the threat is: Try to gauge if the threat is credible, immediate or severe enough to act upon it. Discuss with other healthcare professionals like psychiatrists and supervisors for additional insights.
- Know your ethical and legal boundaries: Make sure to know your organization’s rules about patient confidentiality, mandatory reporting, etc., which will guide your decision-making.
- Collaborate with others: Include psychiatrists, psychologists, social workers or legal experts in your discussions for their unique perspectives on possible interventions while keeping patient rights in mind.
- Discuss consequences with the patient: Have an open conversation with Mr. Anderson about potential risks to others as well as possible legal implications of his threats.
- Involve authorities if needed: If there is an immediate risk to others which can’t be managed internally, report it following proper protocols while sticking to legal obligations.
Scenario: Imagine you’re a nurse in a busy hospital. One day, while giving medicine to your patient, you accidentally give them the wrong amount. Even though nothing bad happens to them right away, you notice your mistake and face a big moral question. Should you tell them about the mistake and risk losing their trust in healthcare, or should you keep quiet to avoid upsetting them?
Ethical Dilemma: As a nurse, your job is to look after the patient’s health and safety. But if you were to reveal a mistake, it might upset the patient, break their trust in healthcare professionals, or even lead to legal problems.
The challenge here is finding the right balance between being honest about mistakes and keeping the patient’s trust. Nurses must think about doing good (beneficence), avoiding harm (non-maleficence), and telling truth (veracity). While open communication is crucial, they also have to weigh how telling might affect the patient emotionally and their view of healthcare.
Telling patients when there has been a mistake is important for many reasons. It respects their freedom of choice by letting them make informed decisions about their care. It’s also good for transparency and helps build trust with your patient because you’re including them in decision-making. However, nurses must be mindful of how they tell patients so as not upset them while fulfilling their ethical duty to report errors.
Solution and Tips: When reporting medical errors, here are some simple tips:
- Admit it: Accept your mistake and take responsibility.
- Check on your patient: See how severe the error might be for the patient. Ask other healthcare professionals or supervisors for advice on understanding what happened.
- Pick the right time and place: Look for somewhere where your patient will feel at ease and won’t be disturbed.
- Speak clearly but kindly: Use simple words instead of medical terms so that they understand what happened. Be kind and let your patient express how they feel.
- Offer solutions: Talk about what can be done to fix any fallout from an error and prevent it from happening again in future.
- Support your patient: Show empathy towards your patient’s feelings or fears related to this incident.
- Follow rules at work: Be sure to follow any rules set by your workplace for reporting errors so that everything is handled properly.
Scenario: Imagine you’re a nurse in a hospital amidst a devastating pandemic. The patients needing critical care far outnumber available resources like ventilators, ICU beds, and medical staff. Now, you’re caught in a difficult ethical dilemma where you have to decide who gets what when the resources are running low.
Ethical Dilemma: In this real-life situation, you face an ethical battle because of limited resources. You have to determine who should get priority based on their survival chances and potential gains from treatments. As a nurse, you have to balance justice, beneficence, and fairness while making these tough calls that could save or end lives.
The ethical challenge here is about equitable distribution of scant resources during a crisis. You have the responsibility of acting in your patients’ best interests but also thinking about the greater good and overall public health impact. In such situations, deciding how to allocate resources can be both emotionally draining and ethically taxing.
You might find yourself asking questions like who should get critical care? Who has better survival odds? How can I ensure everyone gets a fair chance? Your decisions will inevitably affect individual lives, families, and the entire community.
Solution and Tips: To overcome this ethical dilemma of resource allocation during a pandemic, you need an organized approach rooted in ethics. Here are some simplified tips:
- Know your ethical frameworks: Make sure you understand core ethical principles like justice, utility, and proportionality. Use guidelines from professional bodies and healthcare institutions for decision-making during resource scarcity.
- Set up an ethical triage system: Together with an interdisciplinary team, create an equitable triage system considering things like medical urgency, expected outcomes and fair resource distribution.
- Be transparent with communication: Talk openly with patients and their families about allocation challenges. Explain your decision-making process stressing that it’s based on medical facts, ethics and achieving maximum benefits.
- Regularly reassess decisions: Keep reviewing your allocation decisions as conditions change – this could mean altering allocation strategies to uphold fairness while optimizing patient outcomes.
- Fight for more resources: Rally for additional support from healthcare institutions, governments or community at large. Highlighting the effects of resource limitations can help rally support to tackle the crisis.
- Get ethical consultation when needed: When complex decisions arise don’t hesitate to seek guidance from ethics committees or experts ensuring well-balanced perspective.
Working through these steps systematically may help make these hard choices slightly easier for you
Scenario: Imagine you’re a nurse in a palliative care unit. You’ve been taking care of Mr. Thompson, a terminally ill patient, for several weeks. Sadly, his health has considerably worsened and he can’t communicate his end-of-life care preferences anymore. His family members have different views on what should be done next, creating a tough ethical challenge for you.
Ethical Dilemma: The ethical problem here involves decision-making at the end of life. As a nurse, you are drawn between the principles of autonomy, beneficence, and non-maleficence. Your task is to respect Mr. Thompson’s independence while ensuring his well-being and considering the needs and values of his family.
This ethical issue arises because Mr. Thompson’s family members don’t agree on how to handle his end-of-life care. As a nurse, it is your duty to advocate for what’s best for the patient while also taking into account what the family wishes and balancing principles of autonomy and beneficence.
Respecting a patient’s autonomy is crucial but gets tricky when they are no longer able to make decisions themselves. In these situations, you need to work with the patient’s family to ensure their decisions align with any known wishes, values or beliefs expressed by the patient in earlier times. When there are differing opinions within the family, reaching an agreement that respects the patient’s interests can be emotionally taxing as well as ethically challenging.
Solution and Tips: Handling ethical dilemmas like this demands sensitivity, empathy, and open communication. Here are tips to guide you:
- Communicate openly: Make sure all involved feel safe expressing their thoughts and feelings.
- Identify previous wishes: Review any advance directives or living wills left by Mr.Thompson that may guide decision-making.
- Hold Family Meetings: Organize gatherings with all key family members where everyone can share their ideas about prognosis and treatment options.
- Ask Experts: Get advice from ethics committees or palliative care teams who specialize in these situations.
- Promote shared decision-making: Together with the family consider Mr.Thompson’s best interests aiming for consensus respecting his autonomy whilst promoting his well-being.
- Consider Beneficence & Non-Maleficence Principles: Weigh up potential benefits against potential burdens of various treatment options aiming always for maximum comfort dignity quality of life minimum unnecessary suffering.
- Seek Legal Advice if necessary: If disagreements continue getting legal advice will ensure legal obligations are met
Scenario: Put yourself in the shoes of a community healthcare center nurse. One day, a teenage patient named Sarah shares with you that she’s involved in dangerous activities that could harm her and others. She insists you keep this a secret. As a nurse, your duty is to protect everyone from harm, which includes Sarah and anyone her actions might affect. You’re caught in a tough ethical dilemma – do you respect Sarah’s wish for secrecy or prioritize safety?
Ethical Dilemma: In this situation, the ethical problem arises from having to choose between respecting patient confidentiality or ensuring safety – both critical parts of your role as a nurse. The principles of autonomy, beneficence, and non-maleficence guide nursing ethics and require you to find balance between preserving patient privacy and preventing potential harm.
This ethical dilemma revolves around conflicting needs – Sarah’s plea for confidentiality versus the necessity to ensure her safety alongside others’. Nurses should foster trust by maintaining a confidential environment but also need to step in when there’s risk of harm, especially with vulnerable individuals like teenagers.
You must juggle respecting Sarah’s trust while thinking about the potential impacts of her dangerous behaviors. The challenge is figuring out an approach that minimizes harm, maintains confidentiality as much as possible, and still supports Sarah.
Solution and Tips: Solving such an ethical dilemma requires thoughtful deliberation and needs to be focused on the patient. Here are some simple tips:
- Evaluate the risk: Look at how serious or immediate the harm from Sarah’s actions could be. Talk with other healthcare experts like supervisors or mental health specialists for advice.
- Promote open conversation: Provide a safe space where Sarah can talk about her concerns without feeling judged.
- Explain confidentiality limits: Let Sarah know when sharing information might be necessary for preventing harm.
- Get input from other professionals: Seek advice from other experts such as psychiatrists, social workers etc., who can offer different perspectives.
- Ask for informed consent if disclosure is needed: If involving others (like parents or guardians) becomes necessary, discuss this possibility with Sarah first.
- Document everything: Keep detailed records of all decisions made along with their reasons.
- Provide ongoing support: Connect Sarah with resources such as counseling services or support groups.
Remember, it’s crucial for you as a nurse to balance between respecting privacy rights while fulfilling your duties towards safety.
Scenario: Picture this – you’re a nurse in a healthcare setting that’s brimming with multicultural diversity. One day, you find yourself face to face with a situation where one of your patients, Mrs. Rodriguez, insists on relying on her traditional healing methods rather than following the recommended medical treatment. Your challenge here is an ethical one – how do you respect Mrs. Rodriguez’s cultural autonomy while making sure she gets access to safe and effective healthcare?
Ethical Dilemma: What we have here is an ethical quandary. How do you balance between giving due respect to cultural beliefs and pushing for evidence-based healthcare? As a nurse, your guiding principles should be cultural sensitivity, respect for autonomy, benevolence, and non-maleficence. The tricky part is navigating the thin line between respecting cultural diversity and ensuring patient well-being.
The issue boils down to the clash of cultural beliefs against evidence-based healthcare practices. As a nurse, it’s expected of you to deliver patient-centered care that respects and integrates cultural values alongside preferences. However, there’s also your duty as a professional to push for the best possible health outcomes while ensuring patient safety.
In this case, Mrs. Rodriguez’s strong belief in her culture’s healing methods puts you in a spot – how can you accept her beliefs while balancing the need for evidence-based medical interventions? How can you reach a solution that is sensitive towards her culture and respects her autonomy yet ensures she has access to proper healthcare?
Solution and Tips: Finding solutions for such complex ethical dilemmas requires a thoughtful approach. Here are some tips:
- Embrace cultural competence: Understand diverse cultures by learning about their practices, beliefs, and values continually.
- Create trusting relationships: Build trust through open communication with Mrs.Rodriguez by listening actively and asking questions respectfully.
- Collaborate with interpreters or cultural liaisons: If language or culture forms barriers in communication consider getting help from qualified interpreters.
- Educate patients sensitively: Help Mrs.Rodriguez understand the recommended medical treatment in terms of benefits, risks, potential outcomes promoting informed decision-making.
- Promote shared decision-making: Encourage participation from Mrs.Rodriguez’s family so decisions are made considering their beliefs alongside medical recommendations.
- Consultation & support: Seek advice from colleagues or ethicists who can guide through these dilemmas providing valuable perspectives.
- Push for culturally sensitive policies: Advocate developing procedures prioritizing cultural sensitivity along with training programs enhancing understanding among healthcare professionals.
Scenario: Say you’re a nurse in a private healthcare clinic and one day, you stumble onto an ethical challenge. You find out that your colleague, Dr. Wilson, has been prescribing certain medications to patients because he’s getting financial benefits from a pharmaceutical company. As a nurse, you’re meant to look out for your patients’ best interests. Tackling this conflict of interest is tough.
Ethical Dilemma: The main concern here is about conflict of interest in healthcare decisions. As a nurse, ethical principles like integrity, doing good (beneficence), and fairness (justice) guide you. The dilemma emerges when these principles clash with situations that can potentially harm patient care and trust.
This ethical problem surfaces when the doctor’s desire for financial gain clashes with his responsibility to deliver unbiased, patient-oriented care. In such cases, you may wrestle with the potential damage caused by this conflict of interest as it can shake the very foundation of patient trust in healthcare decisions.
Now imagine yourself dealing with this situation – wanting to uphold your nursing ethics while addressing your colleague’s actions. The issue involves standing up for patient welfare, encouraging transparency, and confronting the conflict of interest without damaging team integrity.
Solution and Tips: Addressing conflicts of interest calls for moral courage and devotion towards patient advocacy. Here are some simplified tips:
- Reflect on personal ethics: Think about your own values and professional ethics related to patient care.
- Understand professional guidelines: Get familiar with any codes of ethics or policies about conflicts of interest in your profession.
- Collect information: Gather accurate data about this situation including verbal exchanges or documents related to the financial rewards.
- Talk it over: Discuss it with colleagues or ethics committees who share similar values.
- Take action: If it feels right and aligns with procedures, report it via appropriate channels in your organization – like a supervisor or an ethics committee.
- Promote transparency: Encourage honesty in decision-making within the organization by advocating policy changes that tackle conflicts of interests.
- Stay committed to patients: Keep assessing all decisions from the point-of-view of the patient’s welfare.
Remember managing such conflicts demand continuous vigilance so keep striving to uphold high standards in all aspects.
Scenario: You’re a nurse in a pediatric hospital. One day, you’re asked to help get informed consent for a medical procedure for Ethan, a 10-year-old boy. Ethan’s parents are divorced and can’t agree on whether to go ahead with the procedure. You face an ethical dilemma about informed consent and what’s best for Ethan.
Ethical Dilemma: This real-life situation presents an ethical problem between parental rights, the child’s welfare, and the idea of informed consent. As a nurse, you follow ethical principles like autonomy, doing good (beneficence), and avoiding harm (non-maleficence). You have to handle the difficult task of parental decisions while ensuring Ethan’s well-being.
The ethical problem comes from Ethan’s parents disagreeing about his healthcare choices. As a nurse, you need to think about what’s best for Ethan, respect both parents’ views, and stick to legal rules about getting informed consent from minors. Balancing parents’ rights and children’s rights is tricky in this situation.
In this case, your responsibility is looking out for Ethan’s well-being while making sure his rights are respected. The challenge includes understanding legal and ethical rules for informed consent, helping communication between the parents, and making decisions that focus on what is best for Ethan.
Solution and Tips: To solve this ethical problem about informed consent with kids like Ethan requires careful thought and team work with others involved. Here are some tips:
- Understand legal requirements: Learn local laws about getting informed consent from minors.
- Promote open talk: Help both of Ethan’s parents communicate their concerns openly.
- Focus on the child: Always put the child’s interests first when deciding.
- Get help if needed: If disagreements continue between parents, consider getting help from a mediator or lawyer.
- Ask experts: Get advice from ethics committees or other healthcare workers experienced in children’s ethics.
- Keep records: Keep detailed notes of all talks about decisions made with reasons given.
- Re-evaluate regularly: Keep checking how things are going as new information arrives or situations change.
The goal is always to ensure that decisions taken prioritize Ethan’s welfare above all else.
Scenario: Imagine you’re a nurse in a long-term care facility. One day, you encounter a tricky ethical situation when one of your patients, Mr. Johnson, shows romantic feelings for you. You have to balance professional responsibilities and personal emotions while also addressing Mr. Johnson’s emotional needs. The challenge lies in showing compassion while maintaining professional relationships.
Ethical Dilemma: In this scenario, the ethical issue revolves around keeping professional boundaries intact and preserving the integrity of your relationship with the patient. As a nurse, you are bound by the principles of beneficence, integrity, and professionalism. You need to manage these multiple facets of your role – setting proper boundaries while addressing emotional needs of your patients.
The ethical problem stems from a potential breach in professional boundaries due to Mr. Johnson’s romantic interests towards you. It’s crucial for nurses like yourself to focus on patient care, foster trust, and stick to professional rules. Balancing empathy with appropriate boundary-setting is difficult in such circumstances.
In this situation, you have the responsibility to ensure that your therapeutic relationship remains focused on Mr. Johnson’s healthcare needs while considering his emotional vulnerability. The predicament involves upholding professionalism, outlining clear boundaries without compromising the quality of nursing care provided.
Solution and Tips: To resolve this dilemma about professional boundaries requires careful consideration and commitment to uphold nursing standards:
- Reflect on your responsibilities: Review your own values and duties as a nurse including maintaining boundaries within nurse-patient relationships.
- Set clear boundaries: Communicate openly with Mr.Johnson about the professional nature of your relationship.
- Practice active listening: Show understanding through active listening and empathetic responses that address his emotional needs without crossing any lines.
- Involve others: Consult with other team members or supervisors for guidance or different perspectives.
- Provide resources: Direct Mr.Johnson towards support groups or counseling services beyond what can be given within the confines of the nurse-patient relationship.
- Keep records: Document all interactions accurately as evidence of upholding professional standards.
- Seek ethical consultation if necessary: If things get more complicated or you need further advice, don’t hesitate to consult ethics committees or experts who can provide helpful insights.
The key lies in balancing compassion with professionalism while providing optimal patient care without breaching any ethical or professional boundaries.
Scenario: Imagine you’re a nurse in a children’s clinic. One day, you see injuries on a young patient named Emily that look like she might be being physically abused. Emily trusts you with this secret but pleads with you not to tell anyone, especially her parents. As a nurse, you’re faced with a tough ethical choice of respecting patient confidentiality or reporting suspected child abuse.
Ethical Dilemma: In this situation, the ethical issue is about balancing the need to keep patient information private and the responsibility to protect children from harm. As nurses, your guiding principles include doing good (beneficence), avoiding harm (non-maleficence), and ensuring fairness (justice). The challenge here is finding the right balance between keeping Emily’s secret and fulfilling your duty to keep her safe.
The ethical dilemma here stems from suspecting child abuse and Emily’s request for secrecy. You have to prioritize safety especially for vulnerable individuals like children while also being respectful of their privacy. This calls for maintaining trust while carrying out your duty.
In Emily’s case, it’s about safeguarding her well-being while respecting her secrecy. It’s crucial that you understand the legal requirements for reporting child abuse, communicate sensitively with Emily, and make decisions that are in her best interest.
Solution and Tips: Resolving this ethical dilemma requires kindness and knowledge. Here are some tips:
- Assess risk level: Check how severe or immediate the suspected abuse could be to Emily’s well-being. Speak to other healthcare professionals or child protection services for further insights.
- Speak openly but kindly: Make sure Emily feels safe enough to talk about her experiences and feelings. Explain why it’s important for her safety that the abuse be reported.
- Know your legal duties: Understand local laws around reporting child abuse so you follow them rightly.
- Involve experts: Work closely with child protection services or psychologists who are experts in dealing with cases of suspected child abuse.
- Maintain records: Write down details of any visible injuries or evidence of abuse as well as conversations with Emily which can help during any potential investigation.
- Provide support: Make sure Emily knows she is supported by offering information on counseling services or support groups.
- Take care of yourself: Dealing with suspected cases of child abuse can be emotionally draining so remember to practice self-care and speak about your experiences with colleagues or mental health professionals if needed..
Scenario : imagine you’re a nurse in an oncology ward. One day, you’re assigned to Mr. Anderson, who is terminally ill. He wants to stop life-sustaining treatments and choose palliative care instead. But his family doesn’t agree with his decision; they want him to continue with intensive medical treatments. Now, you’re facing a tough ethical situation: should you respect Mr. Anderson’s autonomy or try to balance the feelings and concerns of his family?
Ethical Dilemma: The dilemma here is about patient autonomy and end-of-life decisions. Nurses follow ethical principles like autonomy, beneficence, and non-maleficence. They must deal with the complicated dynamics of respecting patient autonomy while considering how it affects the patient’s family and their duty to offer compassionate care.
The ethical problem comes from Mr. Anderson’s end-of-life wishes clashing with his family’s opposition. As a nurse, you need to weigh the patient’s autonomy—his right to decide about his own treatment- against the emotional stress and diverse opinions of the family members.
In this situation, your challenge is upholding Mr. Anderson’s autonomy while also managing the concerns and emotions of his loved ones.
Solution and Tips: To solve this tricky problem of patient autonomy and end-of-life decision-making, you’ll need empathy, good communication skills, and teamwork:
- Open up communication: Make sure there’s a safe space for Mr. Anderson and his family where they can share their worries, fears, and hopes without judgment.
- Understand patient wishes: Have thorough discussions with Mr. Anderson so that you understand what he truly wants from his treatment at this stage of life. Explain patients’ rights: Inform the family about patients’ rights in making decisions regarding their own care.
- Promote shared decision-making: Help start discussions where everyone is heard respectfully.
- Seek advice from ethics committees or healthcare professionals: They can guide on how best to handle such complex situations ethically. Offer emotional support as well as counseling services or connect them with appropriate support groups: These resources can help everyone involved deal better emotionally during these challenging times.
- Work closely with other team members like doctors or spiritual guides: An interdisciplinary approach ensures all aspects are covered when advising on treatment decisions.
Remember always that it takes teamwork between healthcare providers, patients, families for best outcomes in such difficult situations.
Scenario: You are a nurse taking care of Emily, a 68-year-old woman who is admitted to the hospital for a severe respiratory infection. You have noticed that Emily seems confused and disoriented, which raises concerns about her ability to make informed decisions about her medical care. After investigating further, you discover that Emily has dementia, and her current mental state is due to the progression of her condition. This presents you with a difficult ethical dilemma regarding autonomy and obtaining informed consent.
Ethical Dilemma: The ethical dilemma in this situation involves balancing respect for Emily’s autonomy with ensuring her well-being as someone with diminished decision-making capacity due to dementia. As a nurse, you must navigate the complex task of upholding patient autonomy while providing necessary care and protection for those who cannot make informed decisions.
The dilemma arises from Emily’s cognitive impairment caused by dementia. You need to consider how much she can participate in decision-making processes and whether she can understand the potential risks, benefits, and alternatives to medical interventions. Striking a balance between respecting autonomy and ensuring her well-being becomes challenging in this situation.
In this case, you face the responsibility of respecting autonomy while also considering what’s best for Emily. The dilemma involves assessing Emily’s capacity for decision-making, involving her family members or legal representatives, and ensuring that her medical care aligns with her values and overall well-being.
Solution and Tips: To resolve this ethical dilemma:
- Evaluate decision-making capacity: Assess Emily’s ability to make decisions by considering her cognitive impairment, fluctuating abilities, and understanding of medical information. Consult with other healthcare professionals for a thorough evaluation.
- Involve family members or legal representatives: Have discussions with Emily’s family members or legal representatives to understand her values and preferences regarding medical care. Collaborate with them to make decisions that are in line with what is best for Emily.
- Use supported decision-making strategies: Explore approaches that involve the patient, family members, and healthcare providers making decisions together in the patient’s best interests. This may include using visual aids or simplified explanations or involving a trusted person who understands Emily’s values and preferences.
- Refer to advance directives or living wills: Review any documents that Emily may have created in the past, such as advance directives or living wills, which can provide guidance on her healthcare preferences.
- Seek ethical consultation: Get guidance from ethics committees or other healthcare professionals experienced in decision-making for patients with dementia. They can offer insights and support to help navigate the challenges and ensure ethical practice.
- Continuously reassess decision-making capacity: Regularly reassess Emily’s ability to make decisions as her cognitive status may change over time. Involve the healthcare team and family members in these evaluations to ensure decisions are made in her best interests.
- Document decision-making processes: Keep accurate and detailed records of all discussions, evaluations, and decisions made regarding Emily’s medical care. This documentation serves as a record of the ethical considerations taken into account and steps taken to ensure her well-being.
By following these steps, you can navigate this complex ethical dilemma while providing the necessary care for Emily, respecting her autonomy as much as possible, and ensuring her overall well-being.
Scenario: You are a nurse working in a busy emergency department. Today, you have been assigned to take care of Mr. Johnson, a 45-year-old man who is experiencing severe pain. The doctor has prescribed a strong pain medication for him, but when you approach Mr. Johnson to give him the medication, he refuses. He is worried about potential side effects and addiction. This puts you in a difficult situation because you want to respect his wishes while also making sure that his pain is managed properly.
Ethical Dilemma: The ethical dilemma here is about respecting patient autonomy and giving medication. As a nurse, you follow the principles of autonomy (letting the patient make decisions), beneficence (doing good for the patient), and non-maleficence (avoiding harm). It’s challenging to balance Mr. Johnson’s right to choose with your responsibility to provide effective care.
The ethical dilemma arises because Mr. Johnson doesn’t want to take the prescribed pain medication because he’s afraid of side effects and addiction. You must respect his right to decide about his own care while considering the consequences of unmanaged pain on his well-being.
Your challenge is finding a way to respect Mr. Johnson’s autonomy while ensuring that he gets adequate pain relief. You’ll need open communication, education about the medication, and addressing his concerns to help him feel comfortable.
Solution and Tips: To solve this ethical dilemma and handle Mr. Johnson’s refusal of medication effectively, follow these tips:
- Open communication: Have a respectful conversation with Mr. Johnson to understand why he refuses the medication. Listen carefully without judgment and acknowledge his right to make decisions.
- Education and addressing concerns: Provide clear information about the prescribed medication, explaining its benefits, possible side effects, and how addiction risks can be managed. Correct any misunderstandings or fears he might have using evidence-based knowledge.
- Exploring alternatives: Discuss other ways to manage his pain, such as non-medication methods or different medications if available. Work with the healthcare team to create a personalized pain management plan that considers Mr. Johnson’s preferences and concerns.
- Respecting autonomy: If, after discussion and education, Mr. Johnson still refuses the medication, respect his decision. Document his informed refusal and make sure he understands the possible consequences of unmanaged pain. Offer ongoing support for his comfort and well-being.
- Involving the healthcare team: Seek input from doctors and pain management specialists by involving them in the decision-making process. Collaborate on a comprehensive approach that balances Mr. Johnson’s autonomy with the goal of effective pain management.
- Assessing and monitoring pain levels: Continuously evaluate Mr. Johnson’s pain levels to ensure they are appropriately managed. Regularly communicate with him to check if the chosen pain management strategies are working well or if adjustments are needed.
- Documentation: Keep accurate records of your discussions, education provided, Mr. Johnson’s concerns, and the agreed-upon pain management plan. This documentation demonstrates adherence to ethical principles and helps with continuity of care.
By following these steps, you can navigate this complex situation ethically while ensuring that Mr. Johnson’s pain is properly managed and that he feels heard and respected in making decisions about his own care.
Scenario: You are a nurse working in a busy hospital during a severe pandemic outbreak. The hospital doesn’t have enough resources like ventilators and intensive care beds to meet the needs of all the patients. You have to make tough decisions about who gets these limited resources.
Ethical Dilemma: The ethical dilemma is about deciding how to distribute limited resources during a pandemic. As a nurse, you have to balance providing good care for everyone with being fair and equal in distributing the resources.
The problem is that there aren’t enough ventilators and intensive care beds for all the patients who need them. You have to decide which patients should get these resources based on their illness severity, chances of getting better, and chance of survival.
Solution and Tips: Your challenge is to provide the best care possible while using the limited resources fairly and equally. The goal is to make decisions that maximize overall patient outcomes while treating everyone fairly.
Here are some tips to help you navigate this difficult situation:
- Set up guidelines: Work with your healthcare team and ethics committees to create rules for distributing resources. Consider things like fairness, overall benefit, and prioritizing those who need it most.
- Use a fair system: Create a transparent process for deciding who gets what resources. Use an objective system that looks at how urgently someone needs help, how sick they are, and their chances of getting better.
- Work together: Get input from doctors, ethicists, administrators, and other healthcare professionals when making decisions. Consider different perspectives so that choices are well-informed and follow the ethical guidelines.
- Be honest with patients: Talk openly with patients and their families about resource shortages. Explain how decisions are made and listen to their concerns. Offer support during this difficult time.
- Review your choices: Regularly check if the resource allocation system is working well. Keep track of patient outcomes and learn from your experiences. Make changes if needed to make the process better.
- Fight for more resources: Advocate for more support from healthcare organizations, policymakers, and the community. Push for strategies that can help reduce shortages, like increasing capacity and public health interventions.
- Take care of yourself: Understand that this situation can be emotionally tough. Take care of yourself by seeking support from colleagues or mental health professionals. Participate in debriefing sessions to process your feelings and prevent burnout.
Scenario: You work as a nurse in a hospice facility that cares for people nearing the end of their lives. One day, you’re assigned to take care of Mr. Chen, an elderly patient with a Chinese cultural background and strong family support. However, you notice that the family’s beliefs about death and dying are different from what’s usually done at the hospice. This puts you in a tough situation where you have to decide between respecting their culture and providing good end-of-life care.
Ethical Dilemma: The ethical dilemma here is about cultural understanding and end-of-life care. As a nurse, it’s important to respect different cultures, let patients make choices for themselves, and give them compassionate care. But sometimes, there can be conflicts between cultural beliefs and the rules we follow in healthcare.
The problem comes from the clash between the family’s beliefs about death and the usual things we do at the hospice. You need to find a way to give culturally appropriate care while also making sure Mr. Chen gets relief from pain, comfort, and support during his final time.
Solution and Tips: To solve this dilemma, try these tips:
- Learn about different cultures: Take time to understand and appreciate diverse practices and values. Learn specifically about how Chinese culture views death, dying, and grieving. Use resources or ask experts for help in becoming more knowledgeable.
- Talk openly with Mr. Chen’s family: Create an environment where they feel comfortable sharing their thoughts without judgment. Listen carefully to their concerns, fears, and wishes regarding end-of-life care.
- Make decisions together: Involve Mr. Chen, his family, and other healthcare team members when deciding what’s best for him. Consider their cultural beliefs along with medical needs like managing pain or providing emotional support.
- Educate gently: Offer sensitive explanations about hospice goals and principles tailored to their culture. Help them understand why pain management, symptom control, and emotional support are important during this time. Clear up any misunderstandings they might have.
- Adjust care within cultural boundaries: Adapt the care plan to respect their cultural beliefs as long as it doesn’t compromise safety or ethical rules. Explore alternative methods of pain relief, spiritual rituals, or ways for family to be involved that align with their culture.
- Get guidance and support: Seek advice from experienced colleagues in cultural understanding or ethics. Consult cultural advisors or interpreters who can help you navigate these challenges. Their expertise can provide valuable insights.
- Reflect on yourself: Continuously think about your own biases, assumptions, and cultural beliefs. Keep learning and being self-aware to improve how you provide patient-centered care to people from different backgrounds.
Scenario: You are a nurse working in a mental health facility. One day, you receive a call from someone claiming to be Sarah’s close friend. They tell you that Sarah has been talking about self-harm and suicide. You now face an ethical dilemma regarding patient confidentiality and the duty to prevent harm.
Ethical Dilemma: As a nurse, you have to balance respecting patient privacy with ensuring their safety. This dilemma arises because you have information about Sarah’s risk of self-harm but need to decide how to handle it while maintaining trust and autonomy.
The challenge is addressing the immediate risk of harm without breaching patient confidentiality or damaging the therapeutic relationship with Sarah. You must make ethical decisions that prioritize her safety while still respecting her trust and autonomy.
Solution and Tips: To navigate this situation:
- Prioritize safety and assess risks carefully: Take the information seriously and evaluate how severe the situation is by considering factors like immediate danger, past self-harm attempts, and available support systems.
- Communicate openly with Sarah: Create a safe space for her to express her thoughts and emotions without revealing what her friend shared directly.
- Build rapport and trust: Show empathy, listen actively, and provide non-judgmental support to establish a trusting relationship with Sarah.
- Involve other healthcare professionals: Seek input from psychologists, psychiatrists, or social workers who can provide different perspectives on managing the risk of self-harm. Collaborate on a comprehensive care plan for Sarah’s safety and mental health needs.
- Respect patient autonomy within limits: Whenever possible, involve Sarah in decisions about her care by discussing potential interventions, explaining recommendations, and seeking her input when feasible.
- Balance confidentiality and duty to warn: Consider legal responsibilities related to duty to warn or protect when there is a high risk of self-harm or harm to others. Consult ethics committees or legal advisors for compliance.
- Document your decision-making process: Maintain accurate records of discussions, assessments, interventions, and referrals related to Sarah’s risk of self-harm. Document the reasons behind your decisions to demonstrate adherence to ethical principles and legal requirements.
Scenario: You are a nurse working in a community healthcare clinic. One of your patients, Mr. Rodriguez, has been diagnosed with a chronic condition that requires consistent adherence to medication and lifestyle modifications. However, during his recent visit, Mr. Rodriguez reveals that he has been non-compliant with his treatment regimen due to personal beliefs and concerns about potential side effects. As a nurse, you find yourself facing a challenging ethical dilemma regarding patient autonomy and the promotion of health outcomes.
Ethical Dilemma: In this situation, you are faced with the ethical dilemma of respecting Mr. Rodriguez’s autonomy while also recognizing the importance of adherence to recommended care for his overall well-being and disease management. Balancing these factors becomes crucial as you navigate through this complex scenario.
Solution and Tips: Resolving the ethical dilemma of patient autonomy and non-adherence to treatment requires effective communication, education, and collaboration. Here are some tips to help you navigate this challenging situation:
- Establish open and non-judgmental communication: Create a safe space where Mr. Rodriguez feels comfortable expressing his concerns and beliefs. Foster open dialogue to understand his reasons for non-adherence and address any misconceptions or fears he may have.
- Explore underlying reasons and beliefs: Engage in discussions to uncover the underlying reasons for Mr. Rodriguez’s non-compliance. Listen attentively and empathetically to gain insight into his beliefs, concerns, and expectations regarding treatment.
- Provide comprehensive education: Offer clear information about the prescribed treatment, its benefits, potential side effects, and long-term consequences of non-adherence. Tailor the education to address Mr. Rodriguez’s specific concerns, providing evidence-based information to alleviate his fears.
- Engage in shared decision-making: Collaborate with Mr. Rodriguez to develop a care plan that considers his beliefs, values, and treatment preferences while balancing optimal health outcomes. Involve him in decision-making processes when appropriate.
- Address barriers and offer support: Identify any barriers contributing to Mr.Rodriguez’s non-adherence and provide resources, tools, or support to help overcome them – such as reminders or referrals to support groups – thus promoting adherence.
- Engage the healthcare team: Collaborate with the healthcare team, including physicians, pharmacists, and other specialists. Discuss Mr. Rodriguez’s concerns, explore alternative treatment options if available, and seek their input and expertise to find solutions that align with his values.
- Continuously assess and reassess: Regularly monitor Mr. Rodriguez’s progress and reassess adherence to the treatment plan. Adapt the care plan as needed based on his evolving beliefs, concerns, and health outcomes. Maintain open communication to address any new challenges that may arise.
By following these tips and approaches, you can navigate this ethical dilemma while striving to respect Mr. Rodriguez’s autonomy and promote his overall well-being in the context of his personal beliefs.
Scenario: You are a nurse in a surgical unit, and one of your patients, Mrs. Thompson, needs a complex surgery for a life-threatening condition. However, you notice that she’s having trouble making decisions because of cognitive decline. This puts you in an ethical dilemma about getting her informed consent while also keeping her safe.
Ethical Dilemma: As a nurse, you face the challenge of obtaining informed consent from Mrs. Thompson when she can’t make clear decisions due to her cognitive decline. You must balance respecting her autonomy with ensuring her safety and well-being.
Solution and Tips: The problem is that Mrs. Thompson can’t fully understand or agree to the surgery because of her cognitive decline. You need to find a way to respect her wishes while protecting her best interests.
To solve this dilemma, you need to assess Mrs. Thompson’s decision-making capacity, involve someone who can make decisions for her (a family member or legal representative), and follow the rules and guidelines for informed consent.
Here are some tips to help you resolve this ethical dilemma:
- Assess decision-making capacity: Evaluate how well Mrs. Thompson can make decisions by considering her cognitive abilities and understanding of the surgery. Get help from experts who specialize in assessing decision-making capacity if needed.
- Involve a surrogate decision-maker: If Mrs.Thompson can’t make decisions, identify someone who can act on her behalf (like a family member or legal representative). Talk to them about Mrs. Thompson’s preferences and values regarding healthcare choices.
- Provide information: Give clear explanations about the surgery, including risks, benefits, and alternatives, to the surrogate decision-maker so they can make an informed choice for Mrs.Thompson.
- Follow rules and guidelines: Make sure you follow all local laws, regulations, and hospital policies related to informed consent for patients with impaired decision-making capacity. Seek advice from ethics committees or legal professionals if necessary.
Scenario: You’re a nurse in a hospital that recently started using electronic health records (EHR). During your shift, a friend from another department asks if they can access the medical records of someone you both know who is currently a patient. This puts you in an ethical dilemma about privacy and keeping patient information confidential in the digital age.
Ethical Dilemma: The problem is deciding how to balance privacy and confidentiality with the new EHR system. As a nurse, you have to follow rules about keeping patient information private. But now you have to figure out how to do that while also dealing with personal relationships at work.
Solution and Tips: You need to protect the patient’s privacy while managing your friend’s expectations. It’s tough because you want to be loyal to your friend, but you also have professional responsibilities and legal obligations.
Here are some tips for resolving this tricky ethical situation:
- Know the rules: Learn about the laws and policies that govern patient privacy and EHR use. Understand what happens if someone accesses patient information without permission.
- Explain why it matters: Talk to your friend about why patient privacy is so important. Help them understand the ethical and legal reasons for not sharing sensitive information. Encourage them to respect boundaries at work.
- Say no politely: Politely decline your friend’s request, making it clear that you can’t share patient information because it goes against professional ethics and legal obligations. Stress that protecting patient privacy is crucial.
- Report if necessary: If your friend keeps asking or if you feel uncomfortable, report the situation to your supervisor or someone higher up in your organization. They can help guide you on what steps to take next and address any breach of confidentiality.
- Promote confidentiality: Encourage a culture of privacy and confidentiality at work by advocating for education on privacy laws and ethical standards for using EHRs. Remind colleagues about their responsibility to keep patient information secure.
- Think about relationships: Consider how personal relationships can affect professional responsibilities. Be mindful of any conflicts of interest and maintain professional boundaries to protect patient privacy and your own integrity.
- Protect information: Take steps to safeguard patient information in the EHR system. Use strong passwords, log out when you’re done, and report any suspicious activity or unauthorized access.
Remember, keeping patient information private is crucial for building trust between patients and healthcare providers. By following ethical guidelines and promoting confidentiality, you can handle this dilemma while staying true to your professional values.

Sophia Miller
Similar posts.

6 Ways to Overcome Interdisciplinary Challenges in…

10 Ways to Build Positive Workplace Culture…

10 Ways to Overcome Communication Barriers in…

10 Ways to Overcome Leadership Challenges in…

Are Male Nurses Attractive?

Can Nurses Wear Rings?
- Career Advancement 29
- Career Transection 20
- Job Satisfaction 16
- Managing Difficult Situations 6
- Work-Life Balance 14
- NCLEX Guide 50
- New Grad Nurse 21
- Nursing Practice Challenges 35
- Work Environment 23
- Emotional Challenges 3
POPULAR POSTS

What Does Baylor Shift Mean?

Can Male Nurses Have Long Hair?

Can You Take a Picture of Your Nurse?

Do School Nurses Wear Scrubs?

Can Nurses Carry Guns?

How Often Do Travel Nurses Get Audited?
- Types of Nursing Degrees and Careers
- Licensed Practical Nurse (LPN/LVN)
- Associate Degree in Nursing (ADN)
- Bachelor of Science in Nursing (BSN)
- Master of Science in Nursing (MSN)
- Doctor of Nursing Practice (DNP)
- Nursing Bridge Programs
- Registered Nurse (RN)
- Nurse Practitioner (NP)
- Certified Registered Nurse Anesthetist (CRNA)
- Certified Nurse Midwife (CNM)
- Certified Nursing Assistant (CNA)
- Certified Medical Assistant (CMA)
- Clinical Nurse Specialist (CNS)
- Pediatric Nurse
- Neonatal Nurse
- Critical Care Nurse
- Psychiatric Nurse
- Forensic Nurse
- Flight Nurse
- Travel Nurse
- Public Health Nurse
- Nurse Administration
- Nursing Informatics
- Nursing Instructor
- Nurse Researcher
- Connecticut
- How to Find the Right Nursing Program
- How to Pay for Nursing School
- Is Nursing For Me?
- Online Resources for Nurses
- Paths to Becoming a Registered Nurse
- How to Pass the NCLEX-RN: 7 Key Tips
- News & Advice
- Nurse Insights
- News & Advice
Nurse Insights: How Do Nurses Approach Ethical Decision-Making?
Written by NursingEducation Staff
April 17, 2024
Ethical decision-making is a crucial aspect of nursing practice. Nurses must navigate complex situations that require balancing the well-being of their patients with their own values and beliefs. In this article, we will explore how nurses approach ethical decision-making, including the guidelines provided by the Code of Ethics for Nurses and the application of the four main ethical principles in daily nursing practice.

How Do Nurses Approach Ethical Decision-Making?
In our Nurse Insights series, experienced nurses offer an insider’s perspective on the nursing profession by addressing common questions, challenges, and triumphs of their careers.
Understanding the Code of Ethics for Nurses
The American Nurses Association (ANA) developed the Code of Ethics for Nurses to provide a standardized set of guidelines for ethical behavior in nursing practice . This Code of Ethics consists of nine provisions and outlines the values, duties, and responsibilities that are inherent to the nursing profession.
Provision 1: Respect for All Individuals
The Code states that you should respect the inherent dignity, worth, and unique attributes of every person, regardless of their health status, race, age, or any other factors. This provision reminds you that every patient deserves respect and good care.
Provision 2: Commitment to the Patient
This provision emphasizes nurses’ primary commitment to the patient, whether it be an individual, family, group, community, or population. It reinforces the importance of loyalty and advocating for the patient’s well-being and safety.
Provision 3: Advocate for and Protect the Rights of the Patient
This provision underscores the importance of advocating for the rights, health, and safety of the patient. You’re expected to safeguard the patient’s privacy and keep them informed about their health situation.
Provision 4: Responsibility and Accountability
This provision highlights your responsibility for individual nursing practice and the requirement to maintain competence. It’s your duty to continually enhance your professional knowledge and skills for the best patient outcomes.
Provision 5: Duty to Provide Optimal Levels of Health Care
As a nurse, you should promote, advocate for, and protect the health, safety, and rights of the patient. This provision includes a mandate for maintaining personal health to ensure the ability to provide optimal care.
Provision 6: Improves Ethical Environment
The Code states that you should establish, maintain, and improve the ethical environment of the work setting to provide safe, quality healthcare.
Provision 7: Advance the Nursing Profession
Provision 7 dictates that you shall advance the nursing profession through research and scholarly inquiry, professional standards development, and the initiation of both nursing and health policy.
Provision 8: Collaboration With Other Health Professionals
You shall collaborate with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
Provision 9: Maintain the Integrity of the Profession
Through professional organizations, the nursing profession must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy.
Following the Code of Ethics in nursing will guide you in making sound decisions in difficult situations. It is an important reference point when dealing with ethical issues, patient rights, and advocacy.
By adhering to these principles, you uphold the integrity of the nursing profession, set an example for other health professionals, and, more importantly, provide the best care for your patients.
Application of Ethical Principles in Nursing Practice
Nurses apply the four ethical principles of autonomy, beneficence, nonmaleficence, and justice in their daily work by respecting patient autonomy, prioritizing patient well-being, avoiding harm, and promoting fairness and equality.
As a nurse, you respect autonomy when you acknowledge that your patients can make their own decisions. It involves understanding and supporting a patient’s decision-making capabilities, meaning you honor their choices even when you might not agree with them. In daily practice, respecting autonomy can mean providing essential information so patients can make informed decisions, seeking their consent before treatments, advocating for patient privacy, and upholding confidentiality.
Beneficence
The principle of beneficence compels you to actively contribute to your patient’s well-being. Practically, beneficence could mean providing effective pain management, ensuring a high standard of personal care, promoting preventive health measures, assisting in rehabilitation, or providing emotional support. The exact application of beneficence often depends on the specific needs of the individual patient.
Nonmaleficence
Nonmaleficence means “doing no harm,” and it is a fundamental principle in nursing. Practically applied, it means you must ensure the care and treatments provided do not knowingly cause harm or pain to your patients. It may involve managing potential side effects, mistakes, or adverse events, and balancing benefits and risks in care decisions.
As a nurse, you apply the principle of justice by treating each patient equally and without bias. This involves ensuring equitable distribution of nursing care and resources, upholding patients’ rights, advocating for your patient’s access to healthcare, and delivering care without discrimination.
The Role of Moral Courage in Nursing Ethics
As a nurse, you will frequently encounter situations where you need to demonstrate moral courage. This is the ability to stand up for what you know is right, even in challenging situations or when faced with adversity. By showing moral courage, you can make sound ethical decisions that respect the dignity, rights, and values of your patients.
Being Courageous in Difficult Situations
Moral courage can involve actions such as advocating for a patient who can’t voice their own needs, refusing to participate in practices that compromise patient care, or speaking up when you observe unethical behavior. This could mean confronting a colleague who isn’t respecting the privacy of a patient, or standing up to a system or protocol that you believe is not in the patient’s best interest. The purpose of moral courage is to safeguard the health and well-being of patients, even when it’s difficult or uncomfortable to do so.
Moral Courage and Ethical Decision-Making
Moral courage directly influences your ethical decision-making processes in nursing. With moral courage, you stand by your professional and personal values, allowing you to navigate complex ethical dilemmas. These dilemmas often have no clear right or wrong answers. For instance, when allocating limited resources, you might need to decide between two equally needy patients. By relying on moral courage, you can make a decision that best upholds the principles of nursing ethics, such as autonomy, beneficence, justice, and non-maleficence.
Moral courage also prevents you from remaining silent or ignoring ethical issues. It pushes you to engage in dialogue, ask hard questions, and explore possible solutions to ethical problems. By doing this, you help create a culture of ethical excellence and patient-centered care in your workplace.
Remember, exercising moral courage can be tough and might lead to stress or emotional fatigue. Therefore, it’s essential to have strategies in place to maintain your resilience and emotional well-being, such as regular debriefs, time for self-reflection, and strong support networks.
Steps in the Ethical Decision-Making Process
Making ethical decisions is an essential part of our lives. However, it can often be challenging to make the right decision. To make an ethical decision, one must follow a set of steps that involve identifying the ethical issue, considering possible actions, evaluating those options, and making a decision. These steps can help ensure that the decision made is fair, just, and aligns with ethical principles.
Step 1: Identify the Ethical Issue
Identifying the ethical issue at hand is the first and most crucial step in the ethical decision-making process. It’s important to take the time to discern whether the situation at hand is indeed an ethical dilemma, or if it is an issue that should be dealt with through a different set of procedures.
Step 2: Gather Information
Once you’ve identified the issue as an ethical one, you should then gather all relevant information. This could include any facts about the situation, the individuals involved, your institutional guidelines, and any legal or professional standards that could apply.
Step 3: Evaluate the Options
A part of ethical decision-making is considering all possible actions in response to the issue. You can evaluate each of these potential actions based on outcomes, potential benefits and harms, legal implications, and alignment with ethical and professional standards.
Step 4: Make a Decision
After carefully considering all the facts and potential actions, it’s time to make a decision. As a nurse, you are guided by the nursing code of ethics and your professional judgment to ensure that your decision best reflects the care and welfare of your patients and aligns with your responsibilities as a nurse.
Step 5: Implement the Decision
Your decision should be implemented in a timely and appropriate manner. You should also communicate your decision to the relevant parties involved, ensuring they understand why this decision was made, and what the next steps will be.
Step 6: Evaluate the Outcome and Reflect
Finally, it’s important to assess the results of your decision. Reflect on whether the outcome was as anticipated and if it adequately resolved the ethical dilemma. This reflective practice will help you learn from the situation and improve your ethical decision-making in the future.
Challenges With Ethical Decision-Making in Nursing
Nursing often involves ethical dilemmas where you will have to make decisions that are in the best interest of your patients. This requires careful thought and consideration of all the relevant ethical principles. One of the main challenges you might face pertains to conflicting ethical principles. For example, you may have to respect a patient’s autonomy, but you must also ensure their well-being.
Balancing Ethical Principles
You might have to choose between patient autonomy and nonmaleficence, which means not causing harm. For example, if a patient doesn’t want a blood transfusion due to personal beliefs, but you know that not getting a transfusion would put their health at risk, this might create an ethical dilemma. A possible solution would be clear and respectful communication to understand your patient’s perspective better, and educating them on the benefits and risks of their decision.
Uncertainty
At times, you may face situations where the best course of action is unclear, such as in end-of-life care or informed consent in diminished capacity cases. At such times, it’s important that you consult with colleagues, professional guidelines, or an ethics committee to gain further insight and clarify doubts.
Cultural Differences
Cultural variations can present significant challenges as well. For example, you may encounter practices and beliefs in certain cultures that are contrary to the conventional healthcare system. It’s crucial that you respect cultural diversity while maintaining a commitment to provide evidence-based care.
Institutional Policies
Your organization’s policies or practices might sometimes not align with your ethical beliefs. If such conflicts arise, engaging in open, respectful dialogue with management or seeking advice from an ethics committee can be helpful.
One of the key strategies to overcome these ethical decision-making challenges is enhancing your ethical competence through continuous education and training, and engaging in reflective practice.
Importance of Continuous Education in Nursing Ethics
The dynamic nature of the healthcare field brings new medical advancements and alterations in policies. Therefore, as a nursing professional, maintaining your learning curve is of great importance. Staying abreast of the latest practices and guidelines is essential in understanding the current best practices in patient care and nursing ethics.
Current Best Practices
Staying updated about the latest best practices in nursing ethics enhances your ability to make sound decisions when ethical dilemmas arise. New or revised guidelines may present innovative approaches to addressing common ethical issues, like patient confidentiality or end-of-life decisions. These insights equip you with the necessary skill set to approach ethical scenarios appropriately, ensuring the utmost respect for a patient’s dignity, autonomy, and well-being.
Interpretation and Application of Ethical Guidelines
Keeping up with new ethical guidelines isn’t sufficient. You must also understand how to interpret and apply these guidelines in real-world scenarios. Continuous learning helps ensure that you can effectively translate theoretical ethical principles into practical action, leading to better patient outcomes and fewer ethical violations.
Fostering a Culture of Ethical Practice
You can serve as role models for nursing students, fellow nurses, and other professionals through your commitment to continuous education and adherence to ethical guidelines. Instilling a culture that promotes ethical practice within your healthcare environment only helps strengthen professional relationships, increasing team harmony and patient satisfaction.
Our Commitment to Accuracy
NursingEducation strives to provide information that is up-to-date and unbiased. By engaging professionals from multiple healthcare perspectives, we ensure our content contains accurate information that helps our readers.
We have combined decades of experience teaching, publishing research, and working with patients in all fields of medicine to create accurate and straightforward online education. Once written, each article undergoes a rigorous peer-review process to bring you the highest quality, most comprehensive content possible.
Our writers receive feedback from reviewers to clarify content, prevent misleading statements, and identify areas that would benefit from more information. Our subject matter experts and reviewers generally work full-time in their professions and work for NursingEducation part-time.

How Can a New Nurse Manage Stress and Burnout?
Read Article

Do Credits From Nursing School Ever Expire?

How Do Nurses Handle Professional Boundaries?
Looking to obtain your nursing degree online.
If you're seeking to gain your pre-licensure degree or advance your professional path, the tuition may be more reasonable than you think. Discover the nursing program that's perfect for you!
Nursing Careers
Nursing degrees.
- Licensed Practical Nurse (LPN)
- Doctorate of Nursing Practice (DNP)
- NCLEX Qbank
- NCLEX Pretest
- NCLEX Categories
- NCLEX Preparation
© 2024 NursingEducation. All Rights Reserved.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Management and Professional Concepts [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2022.

- A new version of this title is available

Nursing Management and Professional Concepts [Internet].
- About Open RN
Chapter 6 – Ethical Practice
6.1. ethical practice introduction, learning objectives.
• Recognize ethical dilemmas and take appropriate action
• Practice in a manner consistent with a code of ethics for nurses
• Compare and contrast theories of ethical decision-making
• Examine resources to resolve ethical dilemmas
• Examine competent practice within the legal/ethical/regulatory framework of health care
• Defend the course of action or give a rationale for the action
• Apply the ANA Code of Ethics to diverse situations in health care
• Analyze the impact of cultural diversity in ethical decision-making
• Identify advocacy as part of the nursing role when responding to ethical dilemmas
The nursing profession is guided by a code of ethics. As you practice nursing, how will you determine “right” from “wrong” actions? What is the difference between morality, values, and ethical principles? What additional considerations impact your ethical decision-making? What are ethical dilemmas and how should nurses participate in resolving them? This chapter answers these questions by reviewing concepts related to ethical nursing practice and describing how nurses can resolve ethical dilemmas. By the end of this chapter, you will be able to describe how to make ethical decisions using the Code of Ethics established by the American Nurses Association.
6.2. BASIC ETHICAL CONCEPTS
The American Nurses Association (ANA) defines morality as “personal values, character, or conduct of individuals or groups within communities and societies,” whereas ethics is the formal study of morality from a wide range of perspectives.[ 1 ] Ethical behavior is considered to be such an important aspect of nursing the ANA has designated Ethics as the first Standard of Professional Performance. The ANA Standards of Professional Performance are “authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.” See the following box for the competencies associated with the ANA Ethics Standard of Professional Performance[ 2 ]:
Competencies of ANA’s Ethics Standard of Professional Performance[ 3 ]
• Uses the Code of Ethics for Nurses with Interpretive Statements as a moral foundation to guide nursing practice and decision-making.
• Demonstrates that every person is worthy of nursing care through the provision of respectful, person-centered, compassionate care, regardless of personal history or characteristics (Beneficence).
• Advocates for health care consumer perspectives, preferences, and rights to informed decision-making and self-determination (Respect for autonomy).
• Demonstrates a primary commitment to the recipients of nursing and health care services in all settings and situations (Fidelity).
• Maintains therapeutic relationships and professional boundaries.
• Safeguards sensitive information within ethical, legal, and regulatory parameters (Nonmaleficence).
• Identifies ethics resources within the practice setting to assist and collaborate in addressing ethical issues.
• Integrates principles of social justice in all aspects of nursing practice (Justice).
• Refines ethical competence through continued professional education and personal self-development activities.
• Depicts one’s professional nursing identity through demonstrated values and ethics, knowledge, leadership, and professional comportment.
• Engages in self-care and self-reflection practices to support and preserve personal health, well-being, and integrity.
• Contributes to the establishment and maintenance of an ethical environment that is conducive to safe, quality health care.
• Collaborates with other health professionals and the public to protect human rights, promote health diplomacy, enhance cultural sensitivity and congruence, and reduce health disparities.
• Represents the nursing perspective in clinic, institutional, community, or professional association ethics discussions.
Reflective Questions
1. What Ethics competencies have you already demonstrated during your nursing education?
2. What Ethics competencies are you most interested in mastering?
3. What questions do you have about the ANA’s Ethics competencies?
The ANA’s Code of Ethics for Nurses with Interpretive Statements is an ethical standard that guides nursing practice and ethical decision-making.[ 4 ] This section will review several basic ethical concepts related to the ANA’s Ethics Standard of Professional Performance, such as values, morals, ethical theories, ethical principles, and the ANA Code of Ethics for Nurses .
Values are individual beliefs that motivate people to act one way or another and serve as guides for behavior considered “right” and “wrong.” People tend to adopt the values with which they were raised and believe those values are “right” because they are the values of their culture. Some personal values are considered sacred and moral imperatives based on an individual’s religious beliefs.[ 5 ] See Figure 6.1 [ 6 ] for an image depicting choosing right from wrong actions.
In addition to personal values, organizations also establish values. The American Nurses Association (ANA) Professional Nursing Model states that nursing is based on values such as caring, compassion, presence, trustworthiness, diversity, acceptance, and accountability. These values emerge from nursing practice beliefs, such as the importance of relationships, service, respect, willingness to bear witness, self-determination, and the pursuit of health.[ 7 ] As a result of these traditional values and beliefs by nurses, Americans have ranked nursing as the most ethical and honest profession in Gallup polls since 1999, with the exception of 2001, when firefighters earned the honor after the attacks on September 11.[ 8 ]
The National League of Nursing (NLN) has also established four core values for nursing education: caring, integrity, diversity, and excellence[ 9 ]:
- Caring: Promoting health, healing, and hope in response to the human condition.
- Integrity: Respecting the dignity and moral wholeness of every person without conditions or limitations.
- Diversity: Affirming the uniqueness of and differences among persons, ideas, values, and ethnicities.
- Excellence: Cocreating and implementing transformative strategies with daring ingenuity.
View the McCombs School of Business Values video on YouTube. [ 10 ]
Morals are the prevailing standards of behavior of a society that enable people to live cooperatively in groups. “Moral” refers to what societies sanction as right and acceptable. Most people tend to act morally and follow societal guidelines, and most laws are based on the morals of a society. Morality often requires that people sacrifice their own short-term interests for the benefit of society. People or entities that are indifferent to right and wrong are considered “amoral,” while those who do evil acts are considered “immoral.”[ 11 ]
Ethical Theories
There are two major types of ethical theories that guide values and moral behavior referred to as deontology and consequentialism.
Deontology is an ethical theory based on rules that distinguish right from wrong. See Figure 6.2 [ 12 ] for a word cloud illustration of deontology. Deontology is based on the word deon that refers to “duty.” It is associated with philosopher Immanuel Kant. Kant believed that ethical actions follow universal moral laws, such as, “Don’t lie. Don’t steal. Don’t cheat.”[ 13 ] Deontology is simple to apply because it just requires people to follow the rules and do their duty. It doesn’t require weighing the costs and benefits of a situation, thus avoiding subjectivity and uncertainty.[ 14 ],[ 15 ],[ 16 ]
The nurse-patient relationship is deontological in nature because it is based on the ethical principles of beneficence and maleficence that drive clinicians to “do good” and “avoid harm.”[ 17 ] Ethical principles will be discussed further in this chapter.
View the McCombs School of Business Deontology video on YouTube. [ 18 ]
Consequentialism is an ethical theory used to determine whether or not an action is right by the consequences of the action. See Figure 6.3 [ 19 ] for an illustration of weighing the consequences of an action in consequentialism. For example, most people agree that lying is wrong, but if telling a lie would help save a person’s life, consequentialism says it’s the right thing to do. One type of consequentialism is utilitarianism. Utilitarianism determines whether or not actions are right based on their consequences with the standard being achieving the greatest good for the greatest number of people.[ 20 ],[ 21 ],[ 22 ] For this reason, utilitarianism tends to be society-centered. When applying utilitarian ethics to health care resources, money, time, and clinician energy are considered finite resources that should be appropriately allocated to achieve the best health care for society.[ 23 ]
Consequentialism
Utilitarianism can be complicated when accounting for values such as justice and individual rights. For example, assume a hospital has four patients whose lives depend upon receiving four organ transplant surgeries for a heart, lung, kidney, and liver. If a healthy person without health insurance or family support experiences a life-threatening accident and is considered brain dead but is kept alive on life-sustaining equipment in the ICU, the utilitarian framework might suggest the organs be harvested to save four lives at the expense of one life.[ 24 ] This action could arguably produce the greatest good for the greatest number of people, but the deontological approach could argue this action would be unethical because it does not follow the rule of “do no harm.”
Watch McCombs School of Business Consequentialism video on YouTube. [ 25 ] Read more about Decision making on organ donation: The dilemmas of relatives of potential brain dead donors.
Interestingly, deontological and utilitarian approaches to ethical issues may result in the same outcome, but the rationale for the outcome or decision is different because it is focused on duty (deontologic) versus consequences (utilitarian).
Societies and cultures have unique ethical frameworks that may be based upon either deontological or consequentialist ethical theory. Culturally-derived deontological rules may apply to ethical issues in health care. For example, a traditional Chinese philosophy based on Confucianism results in a culturally-acceptable practice of family members (rather than the client) receiving information from health care providers about life-threatening medical conditions and making treatment decisions. As a result, cancer diagnoses and end-of-life treatment options may not be disclosed to the client in an effort to alleviate the suffering that may arise from knowledge of their diagnosis. In this manner, a client’s family and the health care provider may ethically prioritize a client’s psychological well-being over their autonomy and self-determination.[ 26 ] However, in the United States, this ethical decision may conflict with HIPAA Privacy Rules and the ethical principle of patient autonomy. As a result, a nurse providing patient care in this type of situation may experience an ethical dilemma. Ethical dilemmas are further discussed in the “ Ethical Dilemmas ” section of this chapter.
See Table 6.2 comparing common ethical issues in health care viewed through the lens of deontological and consequential ethical frameworks.
Ethical Issues Through the Lens of Deontological or Consequential Ethical Frameworks
View in own window
Ethical Principles and Obligations
Ethical principles are used to define nurses’ moral duties and aid in ethical analysis and decision-making.[ 27 ] Although there are many ethical principles that guide nursing practice, foundational ethical principles include autonomy (self-determination), beneficence (do good), nonmaleficence (do no harm), justice (fairness), fidelity (keep promises), and veracity (tell the truth).
The ethical principle of autonomy recognizes each individual’s right to self-determination and decision-making based on their unique values, beliefs, and preferences. See Figure 6.4 [ 28 ] for an illustration of autonomy. The American Nurses Association (ANA) defines autonomy as the “capacity to determine one’s own actions through independent choice, including demonstration of competence.”[ 29 ] The nurse’s primary ethical obligation is client autonomy.[ 30 ] Based on autonomy, clients have the right to refuse nursing care and medical treatment. An example of autonomy in health care is advance directives. Advance directives allow clients to specify health care decisions if they become incapacitated and unable to do so.
Autonomy and Self-Determination
Read more about advance directives and determining capacity and competency in the “ Legal Implications ” chapter.
NURSES AS ADVOCATES: SUPPORTING AUTONOMY
Nurses have a responsibility to act in the interest of those under their care, referred to as advocacy. The American Nurses Association (ANA) defines advocacy as “the act or process of pleading for, supporting, or recommending a cause or course of action. Advocacy may be for persons (whether an individual, group, population, or society) or for an issue, such as potable water or global health.”[ 31 ] See Figure 6.5 [ 32 ] for an illustration of advocacy.
Advocacy includes providing education regarding client rights, supporting autonomy and self-determination, and advocating for client preferences to health care team members and family members. Nurses do not make decisions for clients, but instead support them in making their own informed choices. At the core of making informed decisions is knowledge. Nurses serve an integral role in patient education. Clarifying unclear information, translating medical terminology, and making referrals to other health care team members (within their scope of practice) ensures that clients have the information needed to make treatment decisions aligned with their personal values.
At times, nurses may find themselves in a position of supporting a client’s decision they do not agree with and would not make for themselves or for the people they love. However, self-determination is a human right that honors the dignity and well-being of individuals. The nursing profession, rooted in caring relationships, demands that nurses have nonjudgmental attitudes and reflect “unconditional positive regard” for every client. Nurses must suspend personal judgement and beliefs when advocating for their clients’ preferences and decision-making.[ 33 ]
Beneficence
Beneficence is defined by the ANA as “the bioethical principle of benefiting others by preventing harm, removing harmful conditions, or affirmatively acting to benefit another or others, often going beyond what is required by law.”[ 34 ] See Figure 6.6 [ 35 ] for an illustration of beneficence. Put simply, beneficence is acting for the good and welfare of others, guided by compassion. An example of beneficence in daily nursing care is when a nurse sits with a dying patient and holds their hand to provide presence.
Nursing advocacy extends beyond direct patient care to advocating for beneficence in communities. Vulnerable populations such as children, older adults, cultural minorities, and the homeless often benefit from nurse advocacy in promoting health equity. Cultural humility is a humble and respectful attitude towards individuals of other cultures and an approach to learning about other cultures as a lifelong goal and process.[ 36 ] Nurses, the largest segment of the health care community, have a powerful voice when addressing community beneficence issues, such as health disparities and social determinants of health, and can serve as the conduit for advocating for change.
Nonmaleficence
Nonmaleficence is defined by the ANA as “the bioethical principle that specifies a duty to do no harm and balances avoidable harm with benefits of good achieved.”[ 37 ] An example of doing no harm in nursing practice is reflected by nurses checking medication rights three times before administering medications. In this manner, medication errors can be avoided, and the duty to do no harm is met. Another example of nonmaleficence is when a nurse assists a client with a serious, life-threatening condition to participate in decision-making regarding their treatment plan. By balancing the potential harm with potential benefits of various treatment options, while also considering quality of life and comfort, the client can effectively make decisions based on their values and preferences.
Justice is defined by the ANA as “a moral obligation to act on the basis of equality and equity and a standard linked to fairness for all in society.”[ 38 ] The principle of justice requires health care to be provided in a fair and equitable way. Nurses provide quality care for all individuals with the same level of fairness despite many characteristics, such as the individual’s financial status, culture, religion, gender, or sexual orientation. Nurses have a social contract to “provide compassionate care that addresses the individual’s needs for protection, advocacy, empowerment, optimization of health, prevention of illness and injury, alleviation of suffering, comfort, and well-being.”[ 39 ] An example of a nurse using the principle of justice in daily nursing practice is effective prioritization based on client needs.
Read more about prioritization models in the “ Prioritization ” chapter.
Other Ethical Principles
Additional ethical principles commonly applied to health care include fidelity (keeping promises) and veracity (telling the truth). . An example of fidelity in daily nursing practice is when a nurse tells a client, “I will be back in an hour to check on your pain level.” This promise is kept. An example of veracity in nursing practice is when a nurse honestly explains potentially uncomfortable side effects of prescribed medications. Determining how truthfulness will benefit the client and support their autonomy is dependent on a nurse’s clinical judgment, self-reflection, knowledge of the patient and their cultural beliefs, and other factors.[ 40 ]
A principle historically associated with health care is paternalism. Paternalism is defined as the interference by the state or an individual with another person, defended by the claim that the person interfered with will be better off or protected from harm.[ 41 ] Paternalism is the basis for legislation related to drug enforcement and compulsory wearing of seatbelts.
In health care, paternalism has been used as rationale for performing treatment based on what the provider believes is in the client’s best interest. In some situations, paternalism may be appropriate for individuals who are unable to comprehend information in a way that supports their informed decision-making, but it must be used cautiously to ensure vulnerable individuals are not misused and their autonomy is not violated.
Nurses may find themselves acting paternalistically when performing nursing care to ensure client health and safety. For example, repositioning clients to prevent skin breakdown is a preventative intervention commonly declined by clients when they prefer a specific position for comfort. In this situation, the nurse should explain the benefits of the preventative intervention and the risks if the intervention is not completed. If the client continues to decline the intervention despite receiving this information, the nurse should document the education provided and the client’s decision to decline the intervention. The process of reeducating the client and reminding them of the importance of the preventative intervention should be continued at regular intervals and documented.
Care-Based Ethics
Nurses use a client-centered, care-based ethical approach to patient care that focuses on the specific circumstances of each situation. This approach aligns with nursing concepts such as caring, holism, and a nurse-client relationship rooted in dignity and respect through virtues such as kindness and compassion.[ 42 ],[ 43 ] This care-based approach to ethics uses a holistic, individualized analysis of situations rather than the prescriptive application of ethical principles to define ethical nursing practice. This care-based approach asserts that ethical issues cannot be handled deductively by applying concrete and prefabricated rules, but instead require social processes that respect the multidimensionality of problems.[ 44 ] Frameworks for resolving ethical situations are discussed in the “ Ethical Dilemmas ” subsection of this chapter.
Nursing Code of Ethics
Many professions and institutions have their own set of ethical principles, referred to as a code of ethics , designed to govern decision-making and assist individuals to distinguish right from wrong. The American Nurses Association (ANA) provides a framework for ethical nursing care and guides nurses during decision-making in its formal document titled Code of Ethics for Nurses With Interpretive Statements (Nursing Code of Ethics) . The Nursing Code of Ethics serves the following purposes[ 45 ]:
- It is a succinct statement of the ethical values, obligations, duties, and professional ideals of nurses individually and collectively.
- It is the profession’s nonnegotiable ethical standard.
- It is an expression of nursing’s own understanding of its commitment to society.
The preface of the ANA’s Nursing Code of Ethics states, “Individuals who become nurses are expected to adhere to the ideals and moral norms of the profession and also to embrace them as a part of what it means to be a nurse. The ethical tradition of nursing is self-reflective, enduring, and distinctive. A code of ethics makes explicit the primary goals, values, and obligations of the profession.”[ 46 ]
The Nursing Code of Ethics contains nine provisions. Each provision contains several clarifying or “interpretive” statements. Read a summary of the nine provisions in the following box.
Nine Provisions of the ANA Nursing Code of Ethics
- Provision 1: The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
- Provision 2: The nurse’s primary commitment is to the patient, whether an individual, family, group, community, or population.
- Provision 3: The nurse promotes, advocates for, and protects the rights, health, and safety of the patient.
- Provision 4: The nurse has authority, accountability, and responsibility for nursing practice; makes decisions; and takes action consistent with the obligation to promote health and to provide optimal care.
- Provision 5: The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
- Provision 6: The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
- Provision 7: The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy.
- Provision 8 : The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
- Provision 9: The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy.
Read the free, online full version of the ANA’s Code of Ethics for Nurses With Interpretive Statements.
In addition to the Nursing Code of Ethics, the ANA established the Center for Ethics and Human Rights to help nurses navigate ethical conflicts and life-and-death decisions common to everyday nursing practice.
Read more about the ANA Center for Ethics and Human Rights .
Specialty Organization Code of Ethics
Many specialty nursing organizations have additional codes of ethics to guide nurses practicing in settings such as the emergency department, home care, or hospice care. These documents are unique to the specialty discipline but mirror the statements from the ANA’s Nursing Code of Ethics. View ethical statements of various specialty nursing organizations using the information in the following box.
Ethical Statements of Selected Specialty Nursing Organizations
• American College of Nurse-Midwives
• Emergency Nurses Association
• National Association for Home Care & Hospice
• National Association of Neonatal Nurses
6.3. ETHICAL DILEMMAS
Nurses frequently find themselves involved in conflicts during patient care related to opposing values and ethical principles. These conflicts are referred to as ethical dilemmas. An ethical dilemma results from conflict of competing values and requires a decision to be made from equally desirable or undesirable options.
An ethical dilemma can involve conflicting patient’s values, nurse values, health care provider’s values, organizational values, and societal values associated with unique facts of a specific situation. For this reason, it can be challenging to arrive at a clearly superior solution for all stakeholders involved in an ethical dilemma. Nurses may also encounter moral dilemmas where the right course of action is known but the nurse is limited by forces outside their control. See Table 6.3a for an example of ethical dilemmas a nurse may experience in their nursing practice.
Examples of Ethical Issues Involving Nurses
Read more about Ethics Topics and Articles on the ANA website.
According to the American Nurses Association (ANA), a nurse’s ethical competence depends on several factors[ 1 ]:
- Continuous appraisal of personal and professional values and how they may impact interpretation of an issue and decision-making
- An awareness of ethical obligations as mandated in the Code of Ethics for Nurses With Interpretive Statements [ 2 ]
- Knowledge of ethical principles and their application to ethical decision-making
- Motivation and skills to implement an ethical decision
Nurses and nursing students must have moral courage to address the conflicts involved in ethical dilemmas with “the willingness to speak out and do what is right in the face of forces that would lead us to act in some other way.”[ 3 ] See Figure 6.7[ 4 ] for an illustration of nurses’ moral courage.

Figure 6.12
Moral Courage
Nurse leaders and organizations can support moral courage by creating environments where nurses feel safe and supported to speak up.[ 5 ] Nurses may experience moral conflict when they are uncertain about what values or principles should be applied to an ethical issue that arises during patient care. Moral conflict can progress to moral distress when the nurse identifies the correct ethical action but feels constrained by competing values of an organization or other individuals. Nurses may also feel moral outrage when witnessing immoral acts or practices they feel powerless to change. For this reason, it is essential for nurses and nursing students to be aware of frameworks for solving ethical dilemmas that consider ethical theories, ethical principles, personal values, societal values, and professionally sanctioned guidelines such as the ANA Nursing Code of Ethics.
Moral injury felt by nurses and other health care workers in response to the COVID-19 pandemic has gained recent public attention. Moral injury refers to the distressing psychological, behavioral, social, and sometimes spiritual aftermath of exposure to events that contradict deeply held moral beliefs and expectations.[ 6 ] Health care workers may not have the time or resources to process their feelings of moral injury caused by the pandemic, which can result in burnout. Organizations can assist employees in processing these feelings of moral injury with expanded employee assistance programs or other structured support programs.[ 7 ] Read more about self-care strategies to address feelings of burnout in the “ Burnout and Self-Care ” chapter.
Frameworks for Solving Ethical Dilemmas
Systematically working through an ethical dilemma is key to identifying a solution. Many frameworks exist for solving an ethical dilemma, including the nursing process, four-quadrant approach, the MORAL model, and the organization-focused PLUS Ethical Decision-Making model.[ 8 ] When nurses use a structured, systematic approach to resolving ethical dilemmas with appropriate data collection, identification and analysis of options, and inclusion of stakeholders, they have met their legal, ethical, and moral responsibilities, even if the outcome is less than ideal.
Nursing Process Model
The nursing process is a structured problem-solving approach that nurses may apply in ethical decision-making to guide data collection and analysis. See Table 6.3b for suggestions on how to use the nursing process model during an ethical dilemma.[ 9 ]
Using the Nursing Process in Ethical Situations[ 10 ]
Four-Quadrant Approach
The four-quadrant approach integrates ethical principles (e.g., beneficence, nonmaleficence, autonomy, and justice) in conjunction with health care indications, individual and family preferences, quality of life, and contextual features.[ 11 ] See Table 6.3c for sample questions used during the four-quadrant approach.
Four-Quadrant Approach[ 12 ]
MORAL Model
The MORAL model is a nurse-generated, decision-making model originating from research on nursing-specific moral dilemmas involving client autonomy, quality of life, distributing resources, and maintaining professional standards. The model provides guidance for nurses to systematically analyze and address real-life ethical dilemmas. The steps in the process may be remembered by using the mnemonic MORAL. See Table 6.3d for a description of each step of the MORAL model.[ 13 ],[ 14 ]
PLUS Ethical Decision-Making Model
The PLUS Ethical Decision-Making model was created by the Ethics and Compliance Initiative to help organizations empower employees to make ethical decisions in the workplace. This model uses four filters throughout the ethical decision-making process, referred to by the mnemonic PLUS:
- P: Policies, procedures, and guidelines of an organization
- L: Laws and regulations
- U: Universal values and principles of an organization
- S: Self-identification of what is good, right, fair, and equitable[ 15 ]
The seven steps of the PLUS Ethical Decision-Making model are as follows[ 16 ]:
- Define the problem using PLUS filters
- Seek relevant assistance, guidance, and support
- Identify available alternatives
- Evaluate the alternatives using PLUS to identify their impact
- Make the decision
- Implement the decision
- Evaluate the decision using PLUS filters
6.4. ETHICS COMMITTEES
In addition to using established frameworks to resolve ethical dilemmas, nurses can also consult their organization’s ethics committee for ethical guidance in the workplace. Ethics committees are typically composed of interdisciplinary team members such as physicians, nurses, allied health professionals, administrators, social workers, and clergy to problem-solve ethical dilemmas. See Figure 6.8 [ 1 ] for an illustration of an ethics committee. Hospital ethics committees were created in response to legal controversies regarding the refusal of life-sustaining treatment, such as the Karen Quinlan case.[ 2 ] Read more about the Karen Quinlan case and controversies surrounding life-sustaining treatment in the “ Legal Implications ” chapter.
Ethics Committee
After the passage of the Patient Self-Determination Act in 1991, all health care institutions receiving Medicare or Medicaid funding are required to form ethics committees. The Joint Commission (TJC) also requires organizations to have a formalized mechanism of dealing with ethical issues. Nurses should be aware of the process for requesting guidance and support from ethics committees at their workplace for ethical issues affecting patients or staff.[ 3 ]
Institutional Review Boards and Ethical Research
Other types of ethics committees have been formed to address the ethics of medical research on patients. Historically, there are examples of medical research causing harm to patients. For example, an infamous research study called the “Tuskegee Study” raised concern regarding ethical issues in research such as informed consent, paternalism, maleficence, truth-telling, and justice.
In 1932 the Tuskegee Study began a 40-year study looking at the long-term progression of syphilis. Over 600 Black men were told they were receiving free medical care, but researchers only treated men diagnosed with syphilis with aspirin, even after it was discovered that penicillin was a highly effective treatment for the disease. The institute allowed the study to go on, even when men developed long-stage neurological symptoms of the disease and some wives and children became infected with syphilis. In 1972 these consequences of the Tuskegee Study were leaked to the media and public outrage caused the study to shut down.[ 4 ]
Potential harm to patients participating in research studies like the Tuskegee Study was rationalized based on the utilitarian view that potential harm to individuals was outweighed by the benefit of new scientific knowledge resulting in greater good for society. As a result of public outrage over ethical concerns related to medical research, Congress recognized that an independent mechanism was needed to protect research subjects. In 1974 regulations were established requiring research with human subjects to undergo review by an institutional review board (IRB) to ensure it meets ethical criteria. An IRB is group that has been formally designated to review and monitor biomedical research involving human subjects.[ 5 ] The IRB review ensures the following criteria are met when research is performed:
- The benefits of the research study outweigh the potential risks.
- Individuals’ participation in the research is voluntary.
- Informed consent is obtained from research participants who have the ability to decline participation.
- Participants are aware of the potential risks of participating in the research.[ 6 ]
View a YouTube video discussing Henrietta Lacks, the Tuskegee Experiment, ethics and research. [ 7 ]
6.5. ETHICS AND THE NURSING STUDENT
Nursing students may encounter ethical dilemmas when in clinical practice settings. Read more about research regarding ethical dilemmas experienced by students as described in the box.
Nursing Students and Ethical Dilemmas [ 1 ]
An integrative literature review performed by Albert, Younas, and Sana in 2020 identified ethical dilemmas encountered by nursing students in clinical practice settings. Three themes were identified:
1. Applying learned ethical values vs. accepting unethical practice
Students observed unethical practices of nurses and physicians, such as breach of patient privacy, confidentiality, respect, rights, duty to provide information, and physical and psychological mistreatment, that opposed the ethical values learned in nursing school. Students experienced ethical conflict due to their sense of powerlessness, low status as students, dependence on staff nurses for learning experiences, and fear of offending health care providers.
2. Desiring to provide ethical care but lacking autonomous decision-making
Students reported a lack of moral courage in questioning unethical practices. The hierarchy of health care environments left students feeling disregarded, humiliated, and intimidated by professional nurses and managers. Students also reported a sense of loss of identity in feeling forced to conform their personal identity to that of the clinical environment.
3. Whistleblowing vs. silence regarding patient care and neglect
Students observed nurses performing unethical nursing practices, such as ignoring client needs, disregarding pain, being verbally abusive, talking inappropriately about clients, and not providing a safe or competent level of care. Most students reported remaining silent regarding these observations due to a lack of confidence, feeling it was not their place to report, or the fear of negative consequences. Organizational power dynamics influenced student confidence in reporting unethical practices to faculty or nurse managers.
The researchers concluded that nursing students feel moral distress when experiencing these kinds of conflicts:
- Providing ethical care as learned in their program of study or accepting unethical practices
- Staying silent about patient care neglect or confronting it and reporting it
- Providing quality, ethical care or adapting to organizational culture due to lack of autonomous decision-making
These ethical conflicts can be detrimental to students’ professional learning and mental health. Researchers recommended that nurse educators should develop educational programs to support students as they develop ethical competence and moral courage to confront ethical dilemmas.[ 2 ]
Read more about ethics education in nursing in the ANA’s Online Journal of Issues in Nursing article .
COVID-19 and the Nursing Profession
The COVID-19 pandemic has highlighted the importance of nurses’ foundational knowledge of ethical principles and the Nursing Code of Ethics . Scarce resources in an overwhelmed health care system resulted in ethical dilemmas and moral injury for nurses involved in balancing conflicting values, rights, and ethical principles. Many nurses were forced to weigh their duty to patients and society against their duty to themselves and their families. Challenging ethical issues occurred related to the ethical principle of justice, such as fair distribution of limited ICU beds and ventilators, and ethical dilemmas related to end-of-life issues such as withdrawing or withholding life-prolonging treatment became common.[ 3 ]
Regardless of their practice setting or personal contact with clients affected by COVID-19, nurses have been forced to reflect on the essence of ethical professional nursing practice through the lens of personal values and morals. Nursing students must be knowledgeable about ethical theories, ethical principles, and strategies for resolving ethical dilemmas as they enter the nursing profession that will continue to experience long-term consequences as a result of COVID-19.[ 4 ]
6.6. SPOTLIGHT APPLICATION
A True Story of a New Nurse’s Introduction to Ethical Dilemmas
A new nurse graduate meets Mary, a 70-year-old woman who was living alone at home with Amyotrophic Lateral Sclerosis (ALS or also referred to as “Lou Gehrig’s disease”). Mary’s husband died many years ago and they did not have children. She had a small support system including relatives who lived out of state and friends with whom she had lost touch since her diagnosis. Mary was fiercely independent and maintained her nutrition and hydration through a gastrostomy tube to avoid aspiration.
As Mary’s disease progressed, the new nurse discussed several safety issues related to Mary living alone. As the new nurse shared several alternative options related to skilled nursing care with Mary, Mary shared her own plan. Mary said her plan included a combination of opioids, benzodiazepines, and a plastic bag to suffocate herself and be found by a nurse during a scheduled visit. In addition to safety issues and possible suicide ideation, the new nurse recognized she was in the midst of an ethical dilemma in terms of the treatment plan, her values and what she felt was best for Mary, and Mary’s preferences.
Applying the MORAL Ethical Decision-Making Model to Mary’s Case
6.7. LEARNING ACTIVITIES
Learning activities.
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activities are provided as immediate feedback.)
Ethical Application & Reflection Activity
Filmmaker Lulu Wang first shared a story about her grandmother on This American Life podcast and later turned it into the 2019 movie The Farewell starring Awkwafina. Both share the challenges of a Chinese-born but U.S.-raised woman returning to China and a family who has chosen to not disclose that the grandmother has been given a Stage IV lung cancer diagnosis and three months to live. Listen to the podcast and then answer the following questions:
585: In Defense of Ignorance Act One: What You Don’t Know
1. Reflect on the similarities and differences of your family culture with that of the Billi family. Consider things such as what family gatherings, formal and informal, look like and spoken and unspoken rules related to communication and behavior.
2. The idea of “good” lies and “bad” lies is introduced in the podcast. Nai Nai’s family supports the decision to not tell her about her Stage IV lung cancer, stage a wedding as the excuse to visit and say their goodbyes, and even alter a medical report as good lies necessary to support her mental health, well-being, and happiness. Is the family applying deontological or utilitarian ethics to the situation? Defend your response.
3. Define the following ethical principles and identify examples from this story:
• Autonomy
• Beneficence
• Nonmaleficence
• Paternalism
4. Imagine this story is happening in the United States rather than China and you are the nurse admitting Nai Nai to an inpatient oncology unit. Using the ethical problem-solving model of your choice, identify and support your solution to the ethical dilemma posed when her family requests that Nai Nai not be told that she has cancer.
You are caring for a 32-year-old client who has been in a persistent vegetative state for many years. There is an outdated advanced directive that is confusing on the issue of food and fluids, though clear about not wanting to be on a ventilator if she were in a coma. Her husband wants the feeding tube removed but is unable to say that it would have been the client’s wish. He says that it is his decision for her. Her two adult siblings and parents reject this as a possibility because they say that “human life is sacred” and that the daughter believed this. They say their daughter is alive and should receive nursing care, including feeding. The health care team does not know what to do ethically and fear being sued by either the husband, siblings, or the parents. What do you need to know about this clinical situation? What are the values and obligations at stake in this case? What values or obligations should be affirmed and why? How might that be done?
1. Define the problem.
2. List what facts/information you have.
3. What are the stakeholders’ positions?
• Patient:
• Spouse:
• Family:
• Health Care Team:
• Facility:
• Community:
4. How might the stakeholders’ values differ?
5. What are your values in this situation?
6. Do your values conflict with those of the patient? Describe.

VI. GLOSSARY
The act or process of pleading for, supporting, or recommending a cause or course of action. Advocacy may be for persons (whether an individual, group, population, or society) or for an issue, such as potable water or global health.[ 1 ]
The capacity to determine one’s own actions through independent choice, including demonstration of competence.[ 2 ]
The bioethical principle of benefiting others by preventing harm, removing harmful conditions, or affirmatively acting to benefit another or others, often going beyond what is required by law.[ 3 ]
A set of ethical principles established by a profession that is designed to govern decision-making and assist individuals to distinguish right from wrong.
An ethical theory used to determine whether or not an action is right by the consequences of the action. For example, most people agree that lying is wrong, but if telling a lie would help save a person’s life, consequentialism says it’s the right thing to do.
A humble and respectful attitude towards individuals of other cultures and an approach to learning about other cultures as a lifelong goal and process.
An ethical theory based on rules that distinguish right from wrong.
Conflict resulting from competing values that requires a decision to be made from equally desirable or undesirable options.
Principles used to define nurses’ moral duties and aid in ethical analysis and decision-making.[ 4 ] Foundational ethical principles include autonomy (self-determination), beneficence (do good), nonmaleficence (do no harm), justice (fairness), and veracity (tell the truth).
The formal study of morality from a wide range of perspectives.[ 5 ]
A formal committee established by a health care organization to problem-solve ethical dilemmas.
An ethical principle meaning keeping promises.
A group that has been formally designated to review and monitor biomedical research involving human subjects.
A moral obligation to act on the basis of equality and equity and a standard linked to fairness for all in society.[ 6 ]
The distressing psychological, behavioral, social, and sometimes spiritual aftermath of exposure to events that contradict deeply held moral beliefs and expectations.
Personal values, character, or conduct of individuals or groups within communities and societies.[ 7 ]
The prevailing standards of behavior of a society that enable people to live cooperatively in groups.[ 8 ]
Feelings occurring when an individual is uncertain about what values or principles should be applied to an ethical issue.[ 9 ]
The willingness of an individual to speak out and do what is right in the face of forces that would lead us to act in some other way.[ 10 ]
Feelings occurring when correct ethical action is identified but the individual feels constrained by competing values of an organization or other individuals.[ 11 ]
Feelings occurring when an individual witnesses immoral acts or practices they feel powerless to change.[ 12 ]
The bioethical principle that specifies a duty to do no harm and balances avoidable harm with benefits of good achieved.[ 13 ]
The interference by the state or an individual with another person, defended by the claim that the person interfered with will be better off or protected from harm.[ 14 ]
A type of consequentialism that determines whether or not actions are right based on their consequences, with the standard being achieving the greatest good for the greatest number of people.
Individual beliefs that motivate people to act one way or another and serve as a guide for behavior.[ 15 ]
An ethical principle meaning telling the truth.
Licensed under a Creative Commons Attribution 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/ .
- Cite this Page Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Management and Professional Concepts [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2022. Chapter 6 – Ethical Practice.
- PDF version of this title (18M)
In this Page
- ETHICAL PRACTICE INTRODUCTION
- BASIC ETHICAL CONCEPTS
- ETHICAL DILEMMAS
- ETHICS COMMITTEES
- ETHICS AND THE NURSING STUDENT
- SPOTLIGHT APPLICATION
- LEARNING ACTIVITIES

Other titles in this collection
- Open RN OER Textbooks
Related Items in Bookshelf
- All Textbooks
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Chapter 6 – Ethical Practice - Nursing Management and Professional Concepts Chapter 6 – Ethical Practice - Nursing Management and Professional Concepts
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

Common Ethical Dilemmas in Nursing and their Solutions

Healthcare professionals, including nurses, face ethical dilemmas fairly regularly. Most of the dilemmas are usually serious and very stressful because when faced with a dilemma, a nurse must make a decision, which is easier said than done.
As a nursing student, you might be assigned to write an essay where you identify, analyze, and resolve an ethical dilemma. We have noticed over the years that many students struggle with writing an ethical dilemma nursing essay. If that sounds like you, read this post that comprehensively explores ethical dilemmas in nursing, including their examples and solutions.
In most cases, essays about ethical dilemmas in nursing take the reflective essay approach, where you reflect on real, researched, or imagined clinical scenario or encounter. It could be during your placement, clinical rotations, or shadowing experiences. As you do so, you will borrow from various ethical theories and decision-making models.
If you could use some help, our experienced online nursing essay writers can help you get a bespoke ethical dilemma essay at an affordable fee.
Let's get started with the basics to more advanced concepts.
What is an Ethical Dilemma in Nursing?
An ethical dilemma is a scenario where it is not easy to decide one way or another. Nurses are faced with ethical dilemmas almost every day. They have to make serious and difficult decisions fairly regularly. The decisions can sometimes mean life or death. Therefore, as a student nurse, it is vital to learn about ethical dilemmas nurses face, how to identify them, and how to solve them correctly.
When facing an ethical dilemma, you should always follow the nursing code of ethics . This is because most dilemmas can be solved by following the nursing code of ethics. The nursing code of ethics is a bunch of rules nurses has to follow to provide quality, safe, and unquestionable care to those who need it.
While most dilemmas can be solved by following the code of ethics in nursing, some dilemmas cannot be solved in this manner. The reason is that the nursing code does not guide every ethical dilemma or situation.
If faced with a situation that makes it difficult for you to follow the nursing code of ethics, you should use your judgment to weigh the pros and cons of both decisions to make the right decision.
Examples of ethical dilemmas nurses face regularly include: how to deal with a non-compliant patient, how to deal with a patient that is refusing treatment, and whether to disclose confidential information to help a patient.
Ethical Dilemma Versus Moral Dilemma
The terms ethical and moral are often used interchangeably in speech. However, the two terms do not always mean the same thing. For example, there is a slight difference between ethical and moral dilemmas.
An ethical dilemma involves two morally correct choices, but one is slightly more ethically problematic than the other. In contrast, a moral dilemma is a situation with two morally correct choices, but neither is preferable. For the moral dilemmas, the nurses know the right action yet might be limited to acting by forces outside their control.
As a nurse, you are more likely to face ethical dilemmas than moral dilemmas. Because ethical dilemmas are anticipated, a code of conduct has been created to help you always make the right decision.
Reasons Nurses Face Ethical Dilemmas in Healthcare
There are many reasons why nurses face ethical dilemmas frequently when providing care to patients. The following are the eight main ones:
- Inadequate staffing. When a healthcare facility has fewer staff than it needs to function optimally, nurses sometimes must make a tough decision. They have to decide whether to work longer to care for patients or to prioritize their mental and physical health and work only as much as possible.
- Incompetent peers. As a registered nurse, you will have a big dilemma if you notice a colleague showing incompetence. You will have to choose one of two options to ignore your colleague's incompetence because they are a friend and they probably will not do it again, or report your colleague to a supervisor to ensure high standards are maintained. This is an ethical dilemma since the former is more ethically problematic than the latter.
- Religious/cultural beliefs. Your religious or cultural beliefs may present an ethical dilemma as a practicing nurse. For instance, you might be given a nursing assignment that contradicts your religious beliefs, e.g., you are asked to clean up the private parts of a male patient after a procedure as a Muslim female nurse (this is forbidden according to Islam). It is easy to see how this situation would present an ethical dilemma.
- Patient refusing treatment. There are occasionally situations when patients refuse treatment. As a nurse, you know what is best for the patient. However, you also know that they have the right to make their own decision. So when a patient refuses treatment, this will always present you with an ethical dilemma do you insist and look for ways to ensure they get the treatment or grant them their wish?
- Artificial nutrition and hydration. Some patients and older adults do not want to be fed or hydrated using a tube. This presents a huge ethical dilemma for nurses. This is because nurses are trained to care for people who need it. Therefore, they feel bad about it when they see the need to provide artificial nutrition and hydration and get stopped because of a patient's wishes. They feel so bad because they know there is something they can do, yet they are asked not to do it.
- Providing futile care. Being asked by a patient's family to continue providing care despite a patient's continued decline is one of the biggest ethical dilemmas nurses face. This is especially true for critical care nurses. Being trained medical staff, they can see when it is not in a patient's best interest to continue receiving aggressive interventions. However, most of the time, patient families don't want to give up on their loved ones. Therefore, they insist that interventions continue presenting nurses with a big ethical dilemma.
- Opioid crisis. The opioid crisis across the United States presents nurses with several ethical dilemmas. For example, many nurses do not want to give patients opioid pain medications, especially when they believe they risk getting addicted. Now imagine knowing that a patient can benefit from a medication yet at the same time feeling like it could lead to them getting addicted to it
- Anti-vaccine stance. Nurses who do not mind vaccines face a dilemma whenever they interact with those against vaccines. This is because, on the one hand, they know they have to provide care to everyone without discrimination. Yet, on the other hand, they know that people against vaccines pose a serious public health hazard.
Identifying Ethical Dilemmas in Nursing
As evident in the section above, ethical dilemmas can arise virtually anywhere in the nursing world. It is up to you as a nurse to identify dilemmas when they arise and deal with them as expected by the ANA code of conduct. In this section, we are going to focus on how to identify ethical dilemmas in nursing.
Here are the main indicators of ethical dilemmas in nursing.
- Harm potential. When you face a healthcare situation that has the potential to impact a patient negatively, you are most likely facing an ethical dilemma. If it were so easy to spare the patient from the negative impact, the situation wouldn't be a dilemma because this is the option you would take.
- Conflict of interests. When you face a healthcare situation with a conflict of interests between you and the patient or you and the case management team, it is likely an ethical dilemma.
- Uncertainty. This is perhaps one of the biggest indicators of ethical dilemmas and dilemmas. When you face a healthcare situation in which you are unsure what to decide, you are most likely facing an ethical dilemma. Nurses are trained to judge situations and make decisions quickly. When you cannot do these things as a nurse, something is holding you back, and the situation is likely a dilemma.
- Cautiousness. When you face a healthcare situation in which you are cautious about the outcome of the options you can take, you are most likely facing an ethical dilemma. People are cautious when making ethical dilemma decisions because they do not want to see negative consequences (if any) caused by their decision(s).
- Delay. When you have a decision to make at work and keep delaying the decision-making, you are most likely facing an ethical dilemma. People delay making ethical dilemma decisions because they fear the consequences.
Principles of Nursing Ethics
Principles of nursing ethics were formulated to help nurses consistently make the right decisions when faced with ethical situations. There are many principles of nursing ethics, but the main ones are non-maleficence, beneficence, autonomy, and justice. These are the ones that are always integrated into nursing training programs to help nurses make the right decisions whenever they are faced with difficult situations.
1. Nonmaleficence
Nonmaleficence is probably the most well-known ethical principle in the healthcare world. It applies to nurses, doctors, and other medical professionals.
This principle teaches nurses that it is their responsibility to provide care, treatment options, and/or case management in a manner that does not harm the patient. When you internalize this principle as a nurse, you will always choose to provide care and treat patients safely.
Non-maleficence is an important part of providing patients with safe and quality care. Exercising this principle means doing everything possible as a nurse to provide care while ensuring the highest degree of patient safety.
An excellent example of non-maleficence in nursing practice is withholding the administration of a powerful medication until you get confirmation on whether a patient is allergic to it or not. Another example of maleficence in nursing practice is discontinuing medication when you notice signs of adverse reactions.
When a nurse lacks this principle, it can result in dire consequences for patients. More specifically, a lack of nonmaleficence can lead to reduced patient safety. And, of course, this can mean patient injury or even death. Patient injury or death resulting from lack of nonmaleficence can cause mental trauma, job loss, and even legal consequences.
Therefore, it is imperative to internalize and adhere to this nursing principle.
2. Beneficence
Beneficence is another important nursing principle. This principle is characterized by charity and kindness. It is basically all about ensuring your actions are guided by compassion and maximum consideration of the welfare of those you serve.
While some people choose to pursue nursing for the money or job security, most people in nursing are in it out of their love for serving others. Therefore, this beneficence principle is almost always naturally ingrained in the minds of most nurses.
The best way to apply this nursing ethical principle is to always act in the patient's best interest regardless of the circumstances. Practicing this principle regularly will ensure the patient is always cared for in the best way possible. You will also automatically improve positive patient outcomes.
An excellent example of beneficence in nursing practice is offering to sit with a patient to console them after giving them bad news about their situation. Another superb example of beneficence is drawing curtains to protect a patient's and his family's privacy when exchanging final goodbyes.
Lack of beneficence can result in poor nurse-patient relationships and reduced patient safety. When a patient realizes you are not kind or acting in their best interest, they will not be very interested in showing you kindness or respect. This can result in poor nurse-patient relationships and adverse patient outcomes.
As mentioned above, a lack of beneficence can also lead to reduced patient safety. When you don't act in the patient's best interest, it can lead to safety issues such as failure to record vital info, failure to use protective measures when providing care, and medication errors.
It is easy to see how following this principle can make it easier for nurses to provide quality care and make more ethical decisions.
3. Autonomy
Autonomy is a fundamental nursing ethical principle. It recognizes the right of the patient to make their own decisions. Nurses must never forget this right to avoid imposing their will or self-interest on the patient.
Of course, there is a right way to recognize patients' independence and ability to make their own decisions. This right way involves offering the patient all the necessary information to make the best decisions. This information includes available treatment options and the pros and cons of each option.
Once a nurse has offered a patient all the correct information, they have to respect whatever decisions the patient makes, even if they disagree.
Autonomy is essential in nursing practice because it helps nurses adhere to the patient's wishes. It is also important because it passes responsibility for some major care decisions to the patient they will affect the most.
A good example of autonomy is when a nurse agrees to respect a patient's choice not to get treatment, even if they believe the treatment benefits the patient. Another excellent example of autonomy is a nurse respecting a patient's wish to be seen or attended to by a nurse of the same sex for religious reasons.
When a nurse doesn't practice this ethical principle, they can make decisions that make patients feel disrespected. They can also make decisions that can lead to a breakdown of the nurse-patient relationship. Thus, it is always essential to have this ethical principle in mind.
Justice is a fundamental ethical principle. It is all about nurses showing fairness in the way they provide care. Nurses must provide quality care to patients regardless of their appearance, age, financial history, religious preference, race, and gender.
Even when faced with a situation that involves healthcare for a convicted murderer or any other criminal, a nurse must still offer the best care they can provide.
This nursing ethical principle is crucial because it ensures fairness and equity in nursing. In other words, it provides patients care regardless of who they are. This usually has the effect of making patients feel valued. This, in turn, usually has the effect of enhancing patient outcomes.
A good example of justice in nursing practice is providing care to a known anti-vaccine campaigner when they get COVID or any other vaccine-preventable illness. This is justice and fairness because it allows the person to become well again without considering the negative influence of vaccine use.
A nurse lacking this ethical principle can act in ways that make a patient feel rejected, leading to adverse patient outcomes. It can also lead to unfair prioritization in care provision, resulting in dire consequences for the patient.
By following the nursing ethical principles discussed above and adhering to the ANA code of conduct, you can handle different ethical dilemmas correctly and without serious negative consequences.
Examples of Ethical Dilemmas in Healthcare
Understanding some ethical dilemma scenarios you can write an essay about as a nursing student is essential. Remember, there is never a right or wrong answer; in the same way, there is no small or big ethical issue. As long as it impacts healthcare, it falls within nursing practice or medical ethics.
The following are some of the most common ethical dilemmas in nursing.
1. Pro-choice versus pro-life.
The pro-choice versus pro-life dilemma is common in nursing. For example, when a patient wishes to have an abortion because they do not want a baby, yet a nurse is pro-life because of religious beliefs, it becomes a big dilemma.
SOLUTION : Respect the wishes of the patient.
2. Religious beliefs versus science.
This dilemma is common in nursing practice. For example, it can occur when a patient refuses a specific procedure or treatment because of religious beliefs, yet a nurse knows what science says is best in the situation.
SOLUTION : Respect patient autonomy and do as they wish.
3. Beneficence versus autonomy.
As a nurse, you must practice beneficence (kindness and charity). You are also required to respect the patient's autonomy. Now imagine you have been ordered to give a patient medication to ease pain and suffering, yet they insist on not taking it to stay awake and spend their last minutes with their loved ones. This presents a great beneficence vs. autonomy dilemma.
SOLUTION : Obey the patient's wishes as long as they are conscious and can make their own decisions
4. Anti-vaccine stance.
As a nurse, you must follow exactly what the guardian wants for a child unless it is required by law to do otherwise. Now imagine a situation where a parent refuses to let their child get vaccinated, yet you know at the back of your mind that vaccines benefit children. You know what you must do, yet a guardian insists you must not do it. This is a significant ethical dilemma.
SOLUTION : Obey the guardian's wishes for their child.
5. Withholding information versus being honest.
Nurses are ethically expected to be open and transparent with patients. However, there are cases when you may feel as a nurse that explaining the gravity of a situation to a patient will worsen their stress and anxiety. You may, therefore, think it is more appropriate to withhold some information from them. This presents a big dilemma.
SOLUTION: Always be honest, especially when the situation is complex. Patients deserve to know the truth.
6. Limited resources versus healthcare needs.
Nurses occasionally face situations where their resources are not optimal for the people they serve. Remember the COVID-ventilator issue? Doctors and nurses had to decide whom to give ventilators initially at the start of the pandemic when there were not enough ventilators.
SOLUTION: When the resources are limited, choosing patients based on severity is recommended.
7. Questionable orders.
Doctors and other medical professionals are not perfect. They make mistakes from time to time. Therefore, you will have a big dilemma when a doctor prescribes treatment, and you feel it is not the best treatment in the back of your mind. Do you fulfill the doctor's order or intercede and question it?
SOLUTION: When you feel something wrong is about to happen, you should speak up to protect the patient's interest.
How to Address Ethical Dilemmas in Nursing
The best way to address ethical dilemmas is to internalize and follow the nursing ethical principles and the ANA code of conduct. However, not everyone constantly has the time and energy to review nursing ethical principles and the ANA code of conduct.
For this reason, we have shared the tips below to help you correctly address ethical dilemmas in nursing.
1. A Problem Shared Is a Problem Halved
When you feel uneasy about an ethical situation, you should share it with a trusted colleague or a supervisor. Communicating the problem with someone else invites a fresh perspective to the problem and increases the likelihood of arriving at a better decision.
2. Internalize Patient Autonomy
Remembering and recognizing patient autonomy or the right to make their own decisions is always important. It doesn't matter what you think is best for a patient what they want is what you should do as long as it is legal and within your nursing responsibilities. Of course, you should present the patient with all the information they need to decide. So if you ever have to grapple with an ethical situation that makes you feel like ignoring patient autonomy, you shouldn't do it. You should choose the option that ensures patient autonomy.
3. Respect the Right to Privacy
Every patient has a right to privacy. This means you should treat their information as confidential and only to be shared with them or with persons they approve. It is not in your place to share patient information, especially when it is sensitive. You can only share info when given consent. Therefore, if you ever have a dilemma about sharing information, remember to respect the right to privacy and ask for consent to share info if you think it is necessary.
4. Transparency is Key
You should always be open and honest with patients. Doing this will help you to avoid many ethical situations. It will also make it easy for you to make ethical decisions. Therefore, whenever necessary, please share all the information you can share with patients to help them understand what is happening. Share with them the pros and cons of every treatment or management option. Let them be fully aware of the benefits and risks of everything.
5. Ask Yourself What Is in The Best Interest of the Patient
Whenever you need to make an ethical decision, in addition to all your other considerations, you should ask yourself what is in the patient's best interest. Asking yourself this question will help you act in a way that ensures the patient's best interests are taken into account. It will also force you to involve the patient in decision-making to know what they want or wish for. You can never go wrong by acting in a patient's best interest.
6. Stay Up-To-Date with Ethical Guidelines
Ethical guidelines change regularly. Therefore, to ensure you are always making the right ethical decisions, you should stay up to date with ethical guidelines (both professional guidelines and institution-specific guidelines). It is not always easy to do this, but you can subscribe to nursing blogs that discuss ethical guidelines. This will ensure you always have the latest information you need to make good ethical decisions. You can also stay up to date by enrolling in at least one online ethical nursing training program or course. This will help you to refresh your ethical principles knowledge and to be aware of the latest ethical issues in nursing.
7. Always Do Something as Soon as You Can
When faced with an ethical situation, never do anything and hope the situation will resolve itself. Always do something as soon as possible. This will ensure either the issue is solved or starts getting solved. When you ignore an ethical situation, it has the risk of snowballing and becoming a much bigger issue down the line. Therefore, please do something about an issue whenever you can do it quickly.
8. Negotiating Never Hurts Anybody
One of the best things you can do when facing a nursing ethical dilemma is to negotiate with the parties involved. When you do this respectfully and fairly, you can easily resolve most ethical situations. For example, if a patient refuses a specific treatment for religious reasons, you can convince them to accept it using various persuasion techniques. Of course, you should respect the patient's decision if they insist on a certain stance or position.
9. Talk to Somebody Higher Up
As a nurse, some ethical decisions are not yours; they are above your pay grade. In such a case, they should be referred to somebody higher up, e.g., the nurse manager or the nurse supervisor. Because the manager or supervisor is usually more experienced, they are often in a much better position to handle ethical decisions and teach you what to do when faced with the same situation again.
Consequences of Failing to Address Ethical Dilemmas in Nursing Properly
When you fail to address ethical dilemmas in nursing correctly, there are often negative consequences. The most common negative consequences nurses have to deal with include the following:
1. Loss of License
When you are faced with an ethical decision, you must make sure you act in the way expected of you according to the nursing code of conduct. Failure to act in the manner that is expected of you in the nursing code of conduct can lead to loss of licensure. This is especially true when your decision in an ethical situation is an egregious violation of the nursing code of conduct or the ethical principles of nursing. Therefore, when faced with an ethical decision, it is best to consider the options carefully and to act in the way that is expected of you.
2. Legal Issues
You could face legal issues when you fail to adequately address certain ethical dilemmas in nursing. As a nurse, you have specific responsibilities. You are also expected to adhere to the nursing code of conduct. If you fail to address ethical issues correctly, e.g., you leak confidential information about a celebrity patient for money to the public, you could face legal issues, including a lawsuit and/or criminal charges. Hence it is crucial to think long and hard about some ethical issues before deciding what to do.
3. Job Suspension or Termination
Most hospitals have a code of conduct that nurses and other healthcare professionals must sign when hired. They expect nurses to follow the code to the letter. Most hospitals also expect nurses to follow the ANA code of conduct and to always adhere to the ethical principles of nursing. So when faced with an ethical situation and failing to act correctly, you could end up before the ethics committee of your hospital, and they could recommend your suspension or the termination of your job contract.
4. Stress and Burnout
Ethical situations can cause a lot of stress and mental burnout. They can make it almost impossible for you to continue operating normally. When you ignore them or make the wrong decision, you can potentially make them worse. This can lead to even more stress and even physical burnout. Consequently, it is important to make the right decisions quickly when faced with ethical problems or issues.
5. Negative Patient Outcomes
The worse thing that could happen if you don't address ethical issues correctly is an adverse patient outcome, such as patient deterioration, patient injury, or death. It is always painful for nurses to realize or discover that their decisions caused an adverse patient outcome. It can lead to stress, loss of self-confidence, and so on. Of course, an adverse patient outcome can also lead to legal issues, job suspension, and job loss. So it is best to make the correct decision whenever faced with an ethical dilemma.
Takeaway about Ethical Dilemmas in Nursing Practice
Nursing training is all-rounded in anticipation of all the issues a trained nurse would experience in typical clinical settings. Learning about ethical dilemmas and how to solve them can be a stepping stone toward excellence as a nurse or medical/healthcare practitioner. You will be dealing with many ethical dilemmas in the workplace and an experience on how to solve them can always help you avert adverse situations.
Related Readings:
- List of hot controversial topics for nursing issue papers
If you have an ethical dilemma assignment, paper, essay, or coursework troubling you, you should hire a nursing writer from NurseMyGrade to help you. We are a team of professional nursing writers offering assignment help and coursework help for busy nursing students and nurses worldwide.
Order your nursing paper online right now by filling out the order form. We guarantee 100% original assignments, 100% grammatical correctness, and zero plagiarism.
Struggling with
Related Articles

Writing an Engaging Disusion Post/Response in Nursing School

How to write a PICO(T) Question : A Nurse/Medical Student's Guide

Nursing Theorists and Theories in Nursing Practice
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
Nursing Ethics: Ethical Decision-Making for Nurse Leaders
At a time of unprecedented change, one constant remains: Nurses rate the highest of all professionals for honesty and ethics.
According to a 2019 Gallup poll of U.S. residents, 85% of respondents rated nurses’ ethical standards and honesty as “very high” or “high.” That marked the 18th year in a row that nurses received the highest rating in the survey of consumer impressions of various professions’ ethics. The next highest-rated professions for honesty and ethics were engineers (66%), medical doctors (65%), and pharmacists (64%).
The trust patients put in their nurses has only grown stronger as a result of the ongoing COVID-19 pandemic. A Harris Poll conducted in August 2020 found that 88% of U.S. adults surveyed trust the COVID-19 information they receive from doctors and nurses, compared to 73% who trust information from the U.S. Centers for Disease Control and Prevention (CDC).
Ethics are a cornerstone of the nursing profession. Their importance highlights the role nurses play as advocates for patients’ rights and equitable patient outcomes. This guide explains the genesis of nursing ethics and how nurses put ethics into practice daily to promote the health and well-being of all their patients.
What Are Nursing Ethics?
Ethics are defined as the moral principles that determine how a person or group of people will act or behave in specific situations. Strong ethics are vital to nursing, as moral dilemmas can frequently arise while attending to patients. Nurses and other healthcare professionals must recognize these ethical problems when they occur and apply the profession’s ethics and core values in their judgment and decision-making.
Nursing Ethics and Equitable Care
Health equity’s goal is to ensure that all have the opportunity to “live the healthiest life possible” , as the Robert Wood Johnson Foundation explains, regardless of who they are, where they live, or how much money they make. Daily Nurse describes the four interrelated factors that influence how nurses approach health equity :
- Health disparities are the variations in health and healthcare among segments of the population, including ethnic minorities, immigrants, and people with low income.
- Social determinants of health are the nonmedical and nongenetic factors that account for about 80% of individual health outcomes , according to the National Academy of Medicine.
- Culturally competent healthcare involves respecting and understanding how a segment of the population’s beliefs, language, customs, and behaviors affect disease epidemiology and manifestation. It also considers medication’s effects on various ethnic, cultural, and sexual minorities.
- Social justice highlights nurses’ professional responsibility to respond to systemic injustice and promote and protect human rights.
How Ethics Improve Patient Care Across Demographic Groups
To address health inequity factors, nurses are encouraged to be aware of health disparities that could impair treatment outcomes. They can then refer patients to social workers, case managers, and other healthcare team members for additional services. Nurses should be mindful of the social and economic factors that affect patient and community health.
Trust is key to ensure that patients are comfortable sharing information about their culture and socioeconomic status with nurses and other healthcare professionals. This can be especially challenging when the patient and nurse come from different racial, gender, or ethnic backgrounds.
Principles of Nursing Ethics
Ethical principles are general by nature because they’re intended to serve as a framework that people use to weigh the facts of a situation that presents a moral or an ethical dilemma. The Oncology Nursing Society describes the principles of nursing ethics that serve as guideposts for ethical decision-making in healthcare settings.
Nonmaleficence
Nurses have an obligation not to inflict harm and not to allow others to inflict harm. They must also promote good actions on behalf of their patients. Examples of nonmaleficence are always being truthful to patients and never allowing one patient to be harmed for the benefit of another.
Beneficence
Nurses have a strong duty to act in ways that benefit individuals, communities, and society. Beneficence is rooted in the innate love we feel for humanity and the drive to demonstrate that love through our actions. Beneficence is exemplified by the kindness nurses show their patients in all their interactions and in the willingness to abide by a patient’s wishes, as long as the patient is competent and fully informed.
Nurses must respect their patients at all times, but they’re not required to accept the actions their patients take and the consequences of those actions. Autonomy is the ability to explain one’s needs and make fully informed decisions about one’s health. Illness may threaten a patient’s autonomy. However, nurses are obligated to honor a patient’s autonomous actions.
Nurses are responsible for ensuring that healthcare benefits and burdens are distributed fairly throughout the population. The uneven distribution of healthcare resources is related to societal inequities and personal prejudices. An example is patient triage: when a nurse must decide which of several needy patients requires immediate attention. That decision may depend on where the nurse can do the most good, or where the need is greatest, depending on the nurse’s determination of the most just course of action.
Examples of Nursing Ethics in Action
Technology has impacted healthcare as much as any field, and like other industries, healthcare must address new technologies in ways that don’t threaten patients’ rights and the safety and confidentiality of patient data. These are among the most common ethical dilemmas that nurses face.
Respecting a Patient’s Personal Healthcare Decisions
The concept of self-determination is deeply ingrained in healthcare: As long as patients have sufficient decision-making capacity, they have the right to accept or decline the treatment that their healthcare providers prescribe. As the Journal of Medical Ethics points out, some time must pass between the moment the physician or other healthcare professional determines that some course of action should be taken and the moment the patient is competent enough to decide whether to follow the physician’s advice. Temporizing is the practice of waiting until a patient has sufficient decision-making capacity before advising on the matter.
Being Responsible for Decisions That Result in Suboptimal Care
Nurses make decisions based on the information available to them in the current situation. The more relevant information they have, the more likely their decision will have a positive outcome. When a nurse’s decision leads to a negative outcome, the question becomes: What critical pieces of information were lacking at the time of the decision? Nurses must take responsibility for their decisions and strive to understand why some decisions have negative outcomes.
The Nurse’s Role in End-of-Life Decisions
Early palliative care has been shown to improve the dying experience for patients at the end of their lives as well as for their families. The AMA Journal of Ethics points out the variation in end-of-life care and an underappreciation of the social, political, and cultural issues that underlie decisions about the dying process. The researchers call for a more systemic implementation of communication guidelines for advanced care planning and competent patient-focused end-of-life care.
Following the Nursing Code of Ethics
The American Nurses Association’s nursing code of ethics serves as a guide for nurses to practice with competence and integrity. People’s own set of ethics and morals influence their actions and decision-making, as well as how they perceive the consequences of those actions. In healthcare, ethics allow nurses and other professionals to identify moral dilemmas and apply good judgment to their decisions.
ANA’s nursing code of ethics also ensures that nurses abide by all regulations and policies that apply to their profession and their employment. The code’s nine provisions guide nurses to act ethically in their daily duties and responsibilities. The provisions are based on the four main principles of nursing ethics — nonmaleficence, beneficence, autonomy, and justice — as explained in the book Nursing Ethical Considerations .
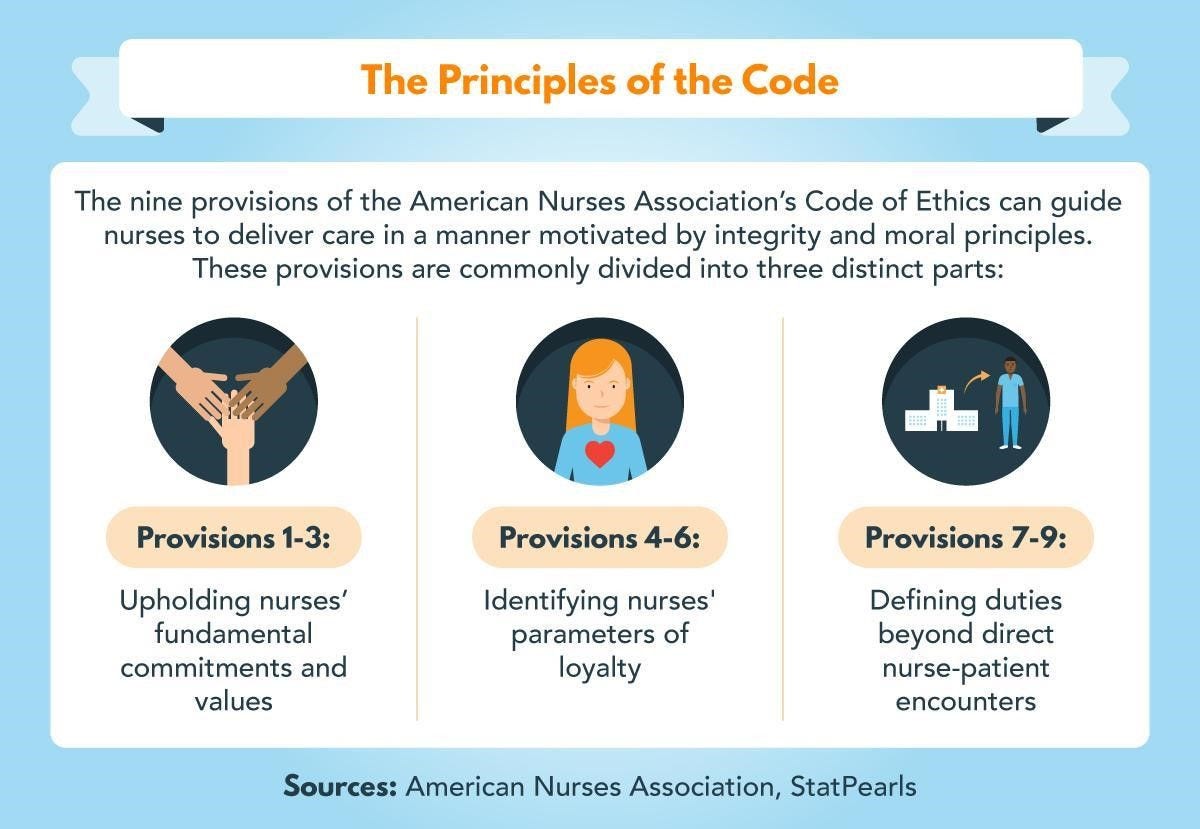
The nine provisions of the American Nurses Association’s Code of Ethics can guide nurses to deliver care in a manner motivated by integrity and moral principles. These provisions are commonly divided into three distinct parts: Provisions 1-3: Upholding nurses’ fundamental commitments and values; Provisions 4-6: Identifying nurses’ parameters of loyalty; and Provisions 7-9: Defining duties beyond direct nurse-patient encounters.
Overview of the ANA Code of Ethics
ANA describes the nursing code of ethics as “non-negotiable in any setting.” The code serves as the foundation for “nursing theory, practice, and praxis” in expressing the “values, virtues, and obligations that shape, guide, and inform nursing as a profession.”
1. Compassion
Nurses recognize the dignity, worth, and uniqueness of all people. They understand that the right to healthcare applies to everyone, and they respect at all times their patients, co-workers, and everyone else they interact with.
2. Commitment
Nurses’ primary commitment is to their patients. They have a duty to recognize and address potential conflicts of interest that may jeopardize their commitment to their patients. This commitment extends to individuals, families, groups, and communities.
3. Advocacy
Nurses promote and protect patients’ rights, health, and safety by understanding privacy guidelines, consent, and the need for full disclosure and honesty when dealing with patients. Misconduct or other threats to patients’ well-being must be reported in a timely manner.
4. Responsibility
Nurses are accountable for the care they provide their patients. They must ensure that their care aligns with professional guidelines, ethical concerns, and patients’ rights.
5. Self-Regard
Nurses must apply the same care standards their patients receive to self-care. Their responsibility to promote health and safety extends beyond the workplace to their homes and other settings. They have a duty to improve and adapt to maintain competence and grow in their profession.
Nurses have a duty to maintain a safe work environment that promotes quality care to all patients. Institutions are responsible for outlining safety standards and enforcing ethical obligations of care to ensure optimal patient outcomes.
7. Healthcare Advancement
In all the roles they play, nurses are charged with advancing the profession through research, development of professional standards, and creation of nursing and health policy. They must ensure that professional practice standards evolve as new healthcare approaches are developed.
8. Human Rights
In collaboration with other healthcare professionals, nurses protect human rights, foster health diplomacy, and address healthcare inequities. As part of this process, nurses are obliged to commit to constant learning and preparation to respond appropriately to novel and unusual situations.
9. Social Justice
Social justice principles must be integrated into a nurse’s practice and advocacy for equitable healthcare policies. By taking part in organizations and committees that acknowledge and address ethics issues, nurses strengthen their voices in calling for social justice.
A Nurse’s Core Values and Commitments
ANA describes the nursing code of ethics as “self-reflective, enduring, and distinctive.”
- It restates the nursing profession’s fundamental values and commitments.
- It identifies the boundaries of duties and loyalty.
- It explains how nurses’ roles extend beyond individual patient interactions.
- It addresses the many relationships nurses have with other healthcare professionals, patients’ families, and the public.
- It makes nurses more aware of the sociopolitical, economic, and environmental context of their profession.
Identifying Duty and Loyalty Boundaries
The fourth, fifth, and sixth principles in the nursing code of ethics address the boundaries that nurses must identify in their work.
- Limits are applied in their personal relationships with patients and co-workers.
- The boundaries can be difficult to maintain because nurses become involved in their patients’ lives at very stressful times.
- Nurses have a duty to ask co-workers and supervisors for help when unsure how to respond to situations that threaten professional boundaries.
A Nurse’s Duties Beyond Patient Care
Advocacy for patients and for healthcare equity extends nurses’ roles into politics and policy. The COVID-19 pandemic has illustrated the often-heroic effort nurses put forth for patients. Michigan Medicine describes how nurses have adapted to new roles and have had their lives turned upside down by the coronavirus.
- Nurses have put together care packages and organized meals for their colleagues to boost morale.
- Reader’s Digest describes how school nurses are creating masks for students and teachers, while other nurses have traveled hundreds or thousands of miles to assist where the need is greatest.
- Home care nurses are finding their roles expand as they comfort their patients, many of whom are older people, as they struggle with isolation during COVID-19 lockdowns, as Fox 13 (KSTU-TV) reports.
Importance of Ethics in Nursing
Until the middle of the 20th century, healthcare ethics received little attention. However, the importance of ethics in nursing came to the fore following World War II, as Medscape explains. The horrors of medical experiments that German doctors conducted during the war led to the Nuremberg Code and the birth of modern medical ethics, as the United States Holocaust Memorial Museum describes.
History of ANA’s Code of Ethics
The need for ethical guidance for healthcare providers was one factor that led to ANA being created in the late 1880s. The first version of the code was adopted in 1950, and the most recent update was published in 2015. The code is continually updated to address changes in the art, science, and practice of nursing and as awareness grows of the link between global health and social, political, and cultural equality.
Nursing Ethics in the Context of Medical Ethics
Medical ethics involve issues that may arise in treating individuals based on values, facts, and logic, as Medscape describes. Doctors in particular face ethical issues that relate to legal and economic issues, such as whether to withhold treatment because of cost, whether to cover up a mistake, or whether to practice defensively to avoid potential malpractice suits.
By contrast, nursing ethics focus on patients’ rights and well-being, the healthcare environment’s safety and quality, and the community’s public health needs. Ultimately the arbiter of what’s ethical in any healthcare situation is the caregiver, in consultation with the patient. Ethical decisions are as integral to patient care as clinical and technical ones.
Ethical Dilemmas Facing Nurses
Even the most extensive code of ethics can’t account for all the potential dilemmas that nurses may encounter in their work. That’s the reason that one of the duties stated in the nursing code of ethics is to seek the advice and counsel of others whenever a nurse is uncertain about a medical decision’s ethical aspects.
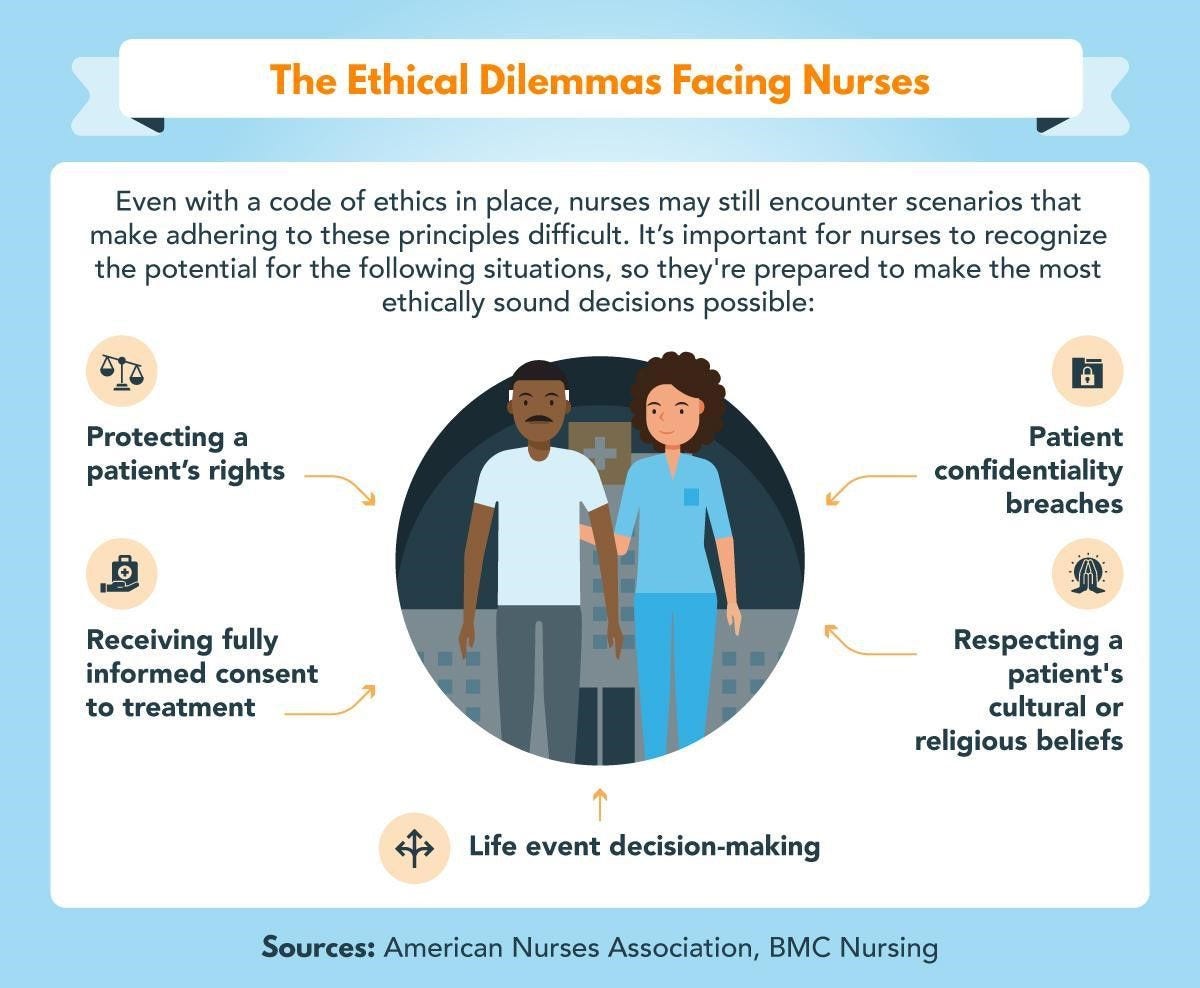
Even with a code of ethics in place, nurses may still encounter scenarios that make adhering to these principles difficult. It’s important for nurses to recognize the potential for the following situations, so they’re prepared to make the most ethically sound decisions possible: protecting a patient’s rights, receiving fully informed consent to treatment, patient confidentiality breaches, respecting a patient’s cultural or religious beliefs, and life event decision-making.
Informed Consent
Nurses must obtain a patient’s informed consent before any medical procedure. As Medical Records Info explains, in addition to explaining all of a procedure’s risks and benefits, nurses must ensure that the patient is sufficiently competent to grant informed consent. Even being medicated can impair a patient’s ability to understand a medical decision’s consequences, which usually means the patient’s family or caretaker will decide on the patient’s behalf.
Protecting Patients’ Rights
Sometimes the advocacy role nurses perform becomes second nature. However, this can cause problems if nurses are overworked or unprepared, despite their best intentions. Advocacy extends to the duty of healthcare administrators to ensure that nurses are working in an environment that allows them to provide patients with the quality care they deserve.
Breaches of Patient Confidentiality
Often a nurse may inadvertently breach patient confidentiality by misunderstanding an action’s consequences. Nurses have a duty to protect sensitive health information, such as medical history, and in the course of dealing with family members, co-workers, and law enforcement officials, they must preserve patient autonomy and avoid oversharing personal information.
Cultural Competency and Nursing Ethics
In recent years, much more attention has been paid to the need for nurses to understand the cultural implications of their interactions with patients. Nurse Advisor highlights the many benefits nurses realize by improving their cultural competence .
- They pay closer attention to the verbal and nonverbal messages that patients and their families send.
- The more contact nurses have with people from different cultures and socioeconomic backgrounds, the higher quality care they can provide as they come to understand new social norms and belief systems.
- By communicating more clearly with patients from diverse backgrounds, nurses engender a sense of trust that allows patients to feel more confident in opening up to healthcare providers.
- As the pace of societal change increases, nurses are better equipped to adapt and modify the care they provide to meet the ever-changing needs of their patients.
Resources on the Importance of Nursing Ethics
- American Nurses Association, Diversity Awareness — Expands on ANA’s social policy statement to address diverse populations’ needs.
- National Association of School Nurses, Cultural Competency Resources — Provides links to sites offering information on becoming culturally sensitive and aware.
- S. National Library of Medicine, “Resources for Ethical Decision Making” — Includes resources on ethics in clinical settings, in home settings, and in perioperative nursing practice.
How Do Ethics Affect Nursing?
The ethical issues that nurses face can increase work-related stress. For example, at Nurse.com, one intensive care unit nurse describes the “moral distress” doctors and nurses feel when a patient’s requests or refusal of treatment are inconsistent with best medical practice and against the patient’s best interest. That nurse sees ethics expressed in the goal of finding the solution that brings about the optimal patient outcome. The solution must also be in line with the patient’s wishes.
Correlating Ethical Patient Care and Optimal Patient Outcomes
Understaffing and other issues beyond a nurse’s control can threaten the responsibility to ensure patient safety. Plos One reports on a study that connected a hospital’s financial performance with its performance in quality and safety analyses . The researchers found that hospitals with the highest financial performance scores had the lowest rates of 30-day readmissions and 30-day mortality, among other quality and safety benefits.
Nurses and other healthcare professionals have little control over their employers’ financial management; yet the responsibility to provide ethical care and treatment as equitably as possible becomes more important when treating disadvantaged populations and those with limited access to healthcare resources.
How Ethics Shape a Nurse’s Daily Responsibilities
Nurses must be aware of the breadth of their responsibilities, and they must determine their readiness to accept those responsibilities. Collegian presents a framework of nurses’ responsibilities where seven domains are intended to promote safety and quality in healthcare.
- Promotion of safety
- Evidence-based practice
- Medical/technical competency
- Person-centered care
- Positive interpersonal behaviors
- Clinical leadership and governance
- Patient perceptions of quality
To validate the domains, researchers solicited nurses’ descriptions of their responsibilities for safe and high-quality care to ensure that nurses’ perceptions match the expectations of their organization and profession.
The Link Between Nurse Ethics and Patient Advocacy
A nurse’s duty to serve as an advocate for patients is stated in the nursing code of ethics’ third provision, as well as in provisions 9.3 and 9.4, which extend patient advocacy outside the workplace to promote social justice in nursing and health policy. Nurse.com explains that advocating for patients includes raising alarms about the climate crisis, food safety, and violence prevention .
ANA encourages nurses to participate in community groups, join neighborhood organizations, or support candidates for local political office. Often it seems progress on matters related to community health comes slowly or not at all, but nurses are trusted and well-respected members of their communities, and their advocacy efforts can be fruitful in many ways.
How Ethics in Nursing Aligns with Ethics in Other Healthcare Professions
The nursing code of ethics closely resembles the American Medical Association’s Code of Medical Ethics , which covers patient-doctor relationships, consent and medical decision-making, privacy, genetics, end-of-life care, and many other issues. A burgeoning area of ethical concern is bioethics, which attempts to promote knowledge and awareness of connections between human life, science, and technology.
Bioethics combines philosophy, theology, history, and law with medical science, emphasizing the application of ethical principles in nursing and health policy. The Center for Practical Bioethics focuses on four domains:
- Aging and end of life
- Clinical and organizational ethics
- Life sciences
- Disparities of health and healthcare
Promoting Ethics in Nurse Education
The earlier nurses begin thinking about nursing ethics, the more aware they become of the importance of integrating ethics into all aspects of the nursing profession. However, a recent study reported in BMC Nursing found that many nursing students minimize the importance of specific ethical values in nursing , such as discussing public policy decisions affecting healthcare funding, and participating in peer reviews.
Just as nurses have many ethical duties to their patients, co-workers, and communities, nurse educators and nurse leaders have a duty to prioritize training nursing students on the importance of ethics in all aspects of nursing practice.
- Doctor of Nursing Practice
Infographic Sources
American Nurses Association, Ethics and Human Rights
BMC Nursing, Increasing Cultural Awareness: Qualitative Study of Nurses’ Perceptions About Cultural Competence Training
StatPearls, Nursing Ethical Considerations

Learn more about our programs.

Take your next step.
Privacy and cookies
We use cookies to give you the best experience on our website. By continuing, you're agreeing to use of cookies. We have recently updated our policy.

Examples of Ethical Dilemmas in Nursing and How to Navigate Them
- Jermaine Huey
- November 29, 2023
Welcome to NursingWriters.net, your trusted source for expert information and guidance on ethical dilemmas in nursing . As a nurse, you encounter numerous situations that require you to make difficult decisions, balancing ethical principles with the well-being of your patients. In this article, we will explore various examples of ethical dilemmas in nursing and provide valuable insights on how to navigate these complex situations.
Key Takeaways:
- Ethical dilemmas are common in nursing and require careful consideration of ethical principles and professional standards.
- Nurses should familiarize themselves with the Nurse’s Code of Ethics to understand their ethical responsibilities.
- An ethical dilemma in nursing occurs when nurses are faced with conflicting choices that challenge their ethical values.
- Common reasons for ethical dilemmas in nursing include patient refusal of treatment , conflicts in personal beliefs, and confidentiality issues.
- Examples of ethical dilemmas in nursing include the clash between pro-life and pro-choice beliefs, conflicts between empirical knowledge and religious beliefs, and balancing patient autonomy with the duty to promote well-being.
Understanding the Nurse’s Code of Ethics
The American Nurses Association (ANA) has established a Code of Ethics for Nurses, which serves as a valuable resource for guiding ethical decision-making in nursing practice. The Nurse’s Code of Ethics outlines the principles and standards that nurses should uphold, ensuring professionalism, integrity, and patient-centered care. By understanding and adhering to these ethical guidelines, nurses can navigate complex situations and provide compassionate and ethical care to their patients.
The Nurse’s Code of Ethics consists of nine provisions that address various aspects of nursing practice. These provisions highlight the importance of treating patients with dignity and respect, advocating for their needs and preferences, and maintaining confidentiality. The Code also emphasizes the significance of lifelong learning, accountability, and collaboration with other healthcare professionals. By following these principles, nurses can promote trust and foster positive relationships with their patients, colleagues, and the broader healthcare system.
Understanding and applying the Nurse’s Code of Ethics is essential for nurses to navigate the ethical challenges they encounter in their practice. By following these ethical guidelines, nurses can ensure the delivery of safe, compassionate, and patient-centered care, upholding the standards of professionalism and integrity that define the nursing profession.
What is an Ethical Dilemma in Nursing?
In the field of nursing, ethical dilemmas are situations where nurses are faced with difficult decisions that involve conflicting values or moral principles . These dilemmas arise when nurses encounter choices that challenge their ethical beliefs or obligations outlined in the Nurse’s Code of Ethics. Ethical dilemmas in nursing require nurses to navigate complex situations that require careful consideration of various factors.
Conflicting values are a central aspect of ethical dilemmas in nursing. Nurses often encounter situations where their personal values may clash with the values of the patient or the ethical principles they are expected to uphold. These dilemmas can create moral distress and tensions between professional responsibilities and personal convictions.
Nursing ethics challenges further add to the complexity of ethical dilemmas. Nurses must navigate the delicate balance between respecting patient autonomy , ensuring beneficence, maintaining confidentiality, and upholding professional accountability. These challenges require critical thinking and ethical decision-making to determine the best course of action in each unique situation.
Overall, ethical dilemmas in nursing are complex situations where nurses must navigate conflicting values , moral principles , and professional obligations. By understanding the definition of ethical dilemmas and the challenges they pose, nurses can develop the skills necessary to make ethical decisions that prioritize patient care and uphold the standards of the nursing profession.
Common Reasons for Ethical Dilemmas in Nursing
Nurses often encounter ethical dilemmas in the course of their practice, and there are several common reasons for these dilemmas. These challenges arise from various situations, including patients refusing treatment , conflicts with personal beliefs, the need for parental consent in pediatric care, the involvement of minors in decision-making, contrasting values between nurses and patients, and confidentiality conflicts .
One common reason for ethical dilemmas is when patients refuse treatment. This can occur when a patient disagrees with the recommended course of action due to personal values, fear, or misinformation. Nurses must navigate this situation by respecting the patient’s autonomy while also considering the potential risks and benefits of the treatment.
Conflicting personal beliefs can also contribute to ethical dilemmas. Nurses may find themselves torn between their professional obligations and their own moral or religious convictions. It is important for nurses to maintain their professional integrity while also recognizing the importance of patient-centered care and respecting diverse perspectives.
Furthermore, the need for parental consent in pediatric care can lead to ethical dilemmas. When parents and healthcare providers have differing opinions on what is in the best interest of the child, nurses must carefully consider legal and ethical frameworks to make informed decisions that prioritize the child’s well-being.
Additionally, the involvement of minors in decision-making can create ethical challenges. Nurses may encounter situations where minors express their own treatment preferences, potentially conflicting with the views of their parents or legal guardians. Balancing the rights of the minor, the authority of the parent, and the ethical principles of autonomy and beneficence can be complex.
Conflicting values between nurses and patients are another common reason for ethical dilemmas. When a nurse’s personal values clash with those of a patient, it is crucial to maintain open communication, empathy, and respect to find a mutually agreeable solution that upholds the patient’s autonomy and promotes their well-being.
Lastly, confidentiality conflicts can contribute to ethical dilemmas in nursing. Nurses are bound by ethical and legal obligations to protect patient privacy, but they may also become aware of potential harm to others, such as self-harm or harm to third parties. This places nurses in a challenging position where they must balance the duty of confidentiality with the duty to protect.
Examples of Ethical Dilemmas in Nursing – Pro-life vs. Pro-choice
One common ethical dilemma in nursing is the clash between pro-life and pro-choice beliefs regarding abortion . This sensitive issue raises questions surrounding patient autonomy, moral conflict , and the nurse’s role in advocating for the best interests of the patient.
“As a nurse, it is essential to approach such situations with empathy and respect for the patient’s values and beliefs while upholding ethical principles and professional responsibilities,” says Mary Thompson, RN, a seasoned nurse with 10 years of experience in obstetrics. “It’s important to remember that our duty as nurses is to provide safe and compassionate care, regardless of personal opinions.”
“Balancing patient autonomy with the nurse’s own ethical framework requires careful consideration and open communication,” explains Thompson. “In the case of a pregnant patient with a history of heart defects who is hesitant to have an abortion due to religious beliefs, it is crucial to engage in meaningful dialogue, thoroughly explain the medical risks, and explore all available options to support the patient in making an informed decision.”
Navigating ethical dilemmas in this context requires sensitivity, adherence to professional guidelines, and a commitment to patient-centered care. It is crucial for nurses to remain non-judgmental, provide emotional support, and advocate for open dialogue between patients, their families, and the healthcare team. By balancing respect for patient autonomy with the nurse’s duty to promote overall well-being, nurses play a vital role in navigating complex ethical dilemmas in the pro-life vs. pro-choice debate.
Additional Resources:
- APA Code of Ethics and Standards for Ethical Practice: https://www.apa.org/ethics/code
- American Nurses Association Ethics and Human Rights: https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/
Examples of Ethical Dilemmas in Nursing – Empirical Knowledge vs. Religious Beliefs
Within the nursing profession, ethical dilemmas often arise when a patient’s religious beliefs come into conflict with empirical knowledge and established medical interventions. This creates a challenging situation for nurses, who must navigate the delicate balance between respecting a patient’s autonomy and ensuring their well-being. A prime example of this ethical dilemma is when a Jehovah’s Witness patient refuses a blood transfusion despite it being medically necessary.
In such a scenario, the nurse is confronted with a moral conflict, as blood transfusions are a widely accepted medical intervention for treating certain conditions. However, Jehovah’s Witnesses have religious beliefs that prohibit them from accepting blood transfusions. The nurse must carefully consider the ethical implications and weigh the patient’s autonomy against the potential risks to their health.
“The challenge lies in finding a solution that respects the patient’s religious beliefs while still fulfilling the nurse’s duty to provide the best possible care.”
Respecting patient autonomy is a fundamental ethical principle in nursing. It requires nurses to involve patients in the decision-making process and honor their preferences and beliefs. However, this ethical dilemma highlights the need for nurses to carefully balance patient autonomy with their duty to provide appropriate medical care based on empirical knowledge and best practices.
Nurses facing this dilemma should engage in open and honest communication with the patient, clarifying their understanding of the religious beliefs and the potential consequences of refusing the recommended medical intervention. The nurse should also involve the healthcare team, seeking guidance and exploring alternative treatment options that align with the patient’s beliefs while ensuring their well-being. Ultimately, the nurse’s role in this ethical dilemma is to facilitate a collaborative decision-making process that respects the patient’s autonomy while upholding the principles of evidence-based practice and patient safety.
Table: Ethical Considerations in the Empirical Knowledge vs. Religious Beliefs Dilemma
This ethical dilemma in nursing highlights the importance of sensitivity, cultural competence, and open communication when navigating conflicts between empirical knowledge and religious beliefs. Nurses must strive to find a balance that respects the patient’s autonomy while ensuring their well-being and adhering to professional ethical standards.
Disclaimer: The scenario presented in this section is fictional and intended for illustrative purposes only. Any resemblance to actual events or individuals is purely coincidental.
Examples of Ethical Dilemmas in Nursing – Autonomy vs. Beneficence
One of the ethical dilemmas frequently faced by nurses is the delicate balance between respecting a patient’s autonomy and promoting their overall well-being. The nurse’s duty to promote the patient’s welfare can sometimes conflict with the patient’s right to make decisions about their own healthcare. This ethical dilemma requires careful consideration and an understanding of the principles of autonomy and beneficence.
For example, imagine a scenario where a patient with diabetes refuses to take insulin, despite it being essential for managing their condition and preventing complications. While the nurse recognizes the importance of promoting the patient’s well-being and preventing harm, they also understand the significance of respecting the patient’s autonomy and their right to make decisions about their own treatment.
In navigating this ethical dilemma, the nurse must engage in open and honest communication with the patient, exploring their concerns and fears. The nurse can provide education and support, emphasizing the potential benefits of insulin therapy while acknowledging the patient’s right to refuse. It is crucial for the nurse to collaborate with the patient, involving them in the decision-making process and empowering them to actively participate in their healthcare.
This table summarizes the key elements of the ethical dilemma between autonomy and beneficence in the context of a patient refusing treatment. It highlights the importance of balancing the patient’s autonomy with the nurse’s duty to promote their overall well-being. By respecting the patient’s autonomy while providing education and support, the nurse can ethically navigate this challenging situation.
Examples of Ethical Dilemmas in Nursing – Confidentiality vs. Duty to Warn
Nurses often face the dilemma of balancing patient confidentiality with the duty to protect others when they become aware of potential harm. This ethical dilemma highlights the tension between respecting a patient’s right to privacy and the responsibility to prevent harm to individuals or the wider community. Let’s explore an example to better understand this dilemma:
A nurse working in a psychiatric facility learns from a patient that they have a plan to harm a specific individual outside of the facility. The patient explicitly requests that the nurse keep this information confidential. The nurse now faces the ethical decision of whether to respect the patient’s right to confidentiality or to breach that trust in order to prevent potential harm to others.
In this scenario, the nurse must carefully consider the ethical principles at play. Patient confidentiality is a fundamental aspect of nursing ethics , emphasizing the importance of trust and maintaining privacy. However, the duty to protect others is equally significant, highlighting the need to prevent harm to individuals in the community. Resolving this ethical dilemma requires a thoughtful and ethical decision-making process.
The nurse should consider consulting the facility’s policies and guidelines regarding confidentiality and duty to warn. They should also engage in discussions with their colleagues, supervisors, and other healthcare professionals to seek guidance and ensure a comprehensive assessment of the situation. Ultimately, the nurse must weigh the potential consequences of maintaining confidentiality against the potential harm that may occur if the information is not shared.
Ethical Considerations in Confidentiality vs. Duty to Warn
The ethical considerations of this dilemma are twofold: maintaining patient confidentiality and ensuring the safety and welfare of others.
- Confidentiality: Respecting patient confidentiality is essential for maintaining trust and preserving patient autonomy. Nurses have a professional and legal obligation to keep patient information confidential, except in situations where there is a clear indication of potential harm to others.
- Duty to Warn: Nurses also have a duty to protect others and prevent harm. If there is a reasonable belief that an individual poses a serious threat to themselves or others, breaching confidentiality may be necessary to ensure the safety and well-being of those at risk.
While the nurse must consider these ethical principles, it is crucial to seek guidance from the facility’s policies and guidelines and engage in meaningful discussions with colleagues and healthcare professionals to make an informed decision. The resolution of this ethical dilemma will depend on careful consideration of the specific circumstances and a commitment to ethical decision-making.
Examples of Ethical Dilemmas in Nursing – End-of-Life Care
End-of-life care presents complex ethical dilemmas for nurses, particularly when balancing a patient’s autonomy with family dynamics and decisions about life-sustaining treatment. One example of an ethical dilemma in end-of-life care is when a patient expresses a desire for a peaceful death without aggressive interventions, while their family wants all possible measures taken.
In such situations, nurses must navigate conflicting values and make decisions that honor both the patient’s autonomy and the family’s concerns. This requires careful consideration of ethical principles such as respect for autonomy, beneficence, and nonmaleficence. Nurses must engage in open and honest communication with the patient and their family, fostering a collaborative approach to decision-making.
When faced with the dilemma of withholding life-sustaining treatment , nurses should prioritize the patient’s autonomy and ensure they have a thorough understanding of their prognosis, treatment options, and potential outcomes. The nurse can provide emotional support and guidance to the patient and their family throughout this difficult process, facilitating discussions about end-of-life goals and preferences.
Table: Ethical Considerations in End-of-Life Care
Nurses play a crucial role in advocating for the patient’s wishes while also providing support to the family during this emotionally challenging time. By addressing end-of-life dilemmas with compassion, empathy, and ethical awareness, nurses can help ensure the best possible care and the preservation of dignity for both the patient and their loved ones.
Ethical dilemmas are an inherent part of nursing practice, requiring nurses to navigate complex situations that may conflict with their personal values or professional obligations. To effectively navigate these challenges, nurses must develop ethical decision-making strategies and cultivate ethical awareness.
By understanding the Nurse’s Code of Ethics and its provisions, nurses can establish a foundation for ethical decision-making. The Code emphasizes the importance of compassion, respect, patient advocacy, professional accountability, and collaboration in nursing practice. These principles can guide nurses in making decisions that prioritize the well-being and autonomy of patients.
Collaboration with healthcare teams, patients, and their families is crucial in resolving ethical dilemmas. By engaging in open and respectful dialogue, nurses can better understand the perspectives and values of all parties involved. This collaborative approach facilitates ethical decision-making that considers the unique circumstances and needs of each situation.
In conclusion, navigating ethical dilemmas in nursing requires a thoughtful and intentional approach. By embracing ethical decision-making strategies , nurses can ensure the ethical responsibilities of their profession are upheld and prioritize the best interests of their patients.
What are some examples of ethical dilemmas in nursing?
Examples of ethical dilemmas in nursing include conflicts between pro-life and pro-choice beliefs regarding abortion , clashes between a patient’s religious beliefs and medical interventions, balancing a patient’s autonomy with their overall well-being, balancing patient confidentiality with the duty to protect others, and decisions regarding end-of-life care .
How can nurses navigate ethical dilemmas in nursing?
Nurses can navigate ethical dilemmas in nursing by considering ethical principles, professional standards, and the Nurse’s Code of Ethics. They should engage in ethical decision-making, understanding the challenges posed by conflicting values and balancing patient autonomy with other considerations.
What is the Nurse’s Code of Ethics?
The Nurse’s Code of Ethics is a set of moral and ethical guidelines established by the American Nurses Association (ANA). It outlines the ethical responsibilities of nurses and emphasizes principles such as compassion, respect, patient advocacy, professional accountability, and collaboration.
What is an ethical dilemma in nursing?
An ethical dilemma in nursing occurs when nurses face difficult decisions that involve conflicting choices, each of which may go against their ethical principles or the Nurse’s Code of Ethics. These dilemmas pose challenges in balancing competing values and making ethical decisions.
Why do nurses encounter ethical dilemmas in their practice?
Nurses may encounter ethical dilemmas in their practice for various reasons, including patients refusing treatment , conflicts with personal beliefs, the need for parental consent in pediatric care, involvement of minors in decision-making, contrasting values between nurses and patients, and conflicts regarding patient confidentiality.
Can you provide an example of an ethical dilemma in nursing related to the pro-life vs. pro-choice debate?
One example of an ethical dilemma in nursing related to the pro-life vs. pro-choice debate is when a pregnant patient with a history of heart defects is hesitant to have an abortion due to religious beliefs. The nurse must navigate the ethical considerations and decision-making process in this situation.
Can you provide an example of an ethical dilemma in nursing related to religious beliefs?
An example of an ethical dilemma in nursing related to religious beliefs is when a Jehovah’s Witness patient refuses a blood transfusion despite it being medically necessary. The nurse must navigate the ethical considerations and decision-making process while respecting the patient’s autonomy and religious beliefs.
Can you provide an example of an ethical dilemma in nursing involving patient autonomy and well-being?
An example of an ethical dilemma in nursing involving patient autonomy and well-being is when a patient with diabetes refuses to take insulin. The nurse must navigate the ethical considerations and decision-making process while respecting the patient’s autonomy but also ensuring their overall well-being.
Can you provide an example of an ethical dilemma in nursing involving patient confidentiality and duty to protect others?
An example of an ethical dilemma in nursing involving patient confidentiality and duty to protect others is when a nurse learns about a patient’s plan to cause harm to someone else. The nurse must navigate the ethical considerations and decision-making process, weighing the importance of patient confidentiality against the duty to protect others.
Can you provide an example of an ethical dilemma in nursing related to end-of-life care?
An example of an ethical dilemma in nursing related to end-of-life care is when a patient expresses a desire for a peaceful death without aggressive interventions, while their family wants all possible measures taken. The nurse must navigate the ethical considerations and decision-making process, taking into account patient autonomy and family dynamics .
Have a subject expert Write for You Now
Have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, table of contents.
- Our Guarantees
- Client Reviews
- Privacy Policy
- Terms and Conditions
Knowledge Base
- All Writing Guides
- Nursing Essay Writing Guides
- Topics Ideas
- Nursing Guides
- Nursing Exemplar Papers
- DNP Nursing Paper Examples
- MSN Nursing Paper Writing
Nursing Writers Service
- Write My Nursing Paper
- Nursing Paper Writers
- Nursing Assignment Writers
- Nursing research paper writers
- Nursing Paper Writing Services
- Online Nursing Papers
- Personal Nursing Philosophy Paper
- Nursing Paper Writing Services reviews
- Nursing School Paper Writing Service
- Nursing Research Paper Writing Service
- Nursing Paper Writing Service
- Research Paper Writing Service nurses
- Paper Writing Service Nursing
- Paper Writing Service Reddit nursing
- Paper Writing Service chamberlain nursing
Writing Tools
- Citation Generator
- Topic Generator
- Thesis Generator
- Sentence Rewriter
- Title Page Generator
- Research Paper Title Generator
Use our resources and guides to write perfect papers. You can use our writing service and order customized sample papers without plagiarism!
Disclaimer
NursingWriters.net helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.

✍️ Nursing Writers
Typically replies within minutes
Hey! 👋 Need help with an assignment?
WhatsApp Us
🟢 Online | Privacy policy
WhatsApp us

IMAGES
COMMENTS
3. Nurses who avoid ethical dilemmas could lose their jobs. Depending on the situation, failure to address an ethical dilemma in nursing could result in consequences such as a reprimand from management or loss of a job. 4. Loss of licensure: There are some ethical dilemmas in nursing that have severe consequences when avoided.
Aug 11, 2023 · Consider Ethical Decision-Making Frameworks: Use the ethical principles of fairness and justice in the nursing code of ethics to guide the nurse’s actions. By considering factors like the potential benefits, risks, and overall impact on patients and the community, the nurse can strive to allocate resources in an equitable and ethical manner.
For example, Provision 1.4 of the American Nurses Association (ANA) Code of Ethics for Nurses with Interpretive Statements (the Code) states that the patient has a right to self-determination. In the clinical setting, ethical conflicts related to self-determination and other ethical principles are not unusual.
Ethical Dilemma: The ethical dilemma in this situation involves balancing respect for Emily’s autonomy with ensuring her well-being as someone with diminished decision-making capacity due to dementia. As a nurse, you must navigate the complex task of upholding patient autonomy while providing necessary care and protection for those who cannot ...
Apr 17, 2024 · Steps in the Ethical Decision-Making Process. Making ethical decisions is an essential part of our lives. However, it can often be challenging to make the right decision. To make an ethical decision, one must follow a set of steps that involve identifying the ethical issue, considering possible actions, evaluating those options, and making a ...
The ANA’s Code of Ethics for Nurses with Interpretive Statements is an ethical standard that guides nursing practice and ethical decision-making. This section will review several basic ethical concepts related to the ANA’s Ethics Standard of Professional Performance, such as values, morals, ethical theories, ethical principles, and the ANA ...
Jun 10, 2023 · Principles of Nursing Ethics. Principles of nursing ethics were formulated to help nurses consistently make the right decisions when faced with ethical situations. There are many principles of nursing ethics, but the main ones are non-maleficence, beneficence, autonomy, and justice.
Utilizing the ethical principles of autonomy, beneficence, nonmaleficence, fidelity, justice, and paternalism as outlined by the American Nurses Association (ANA) provides us with a firm foundation for ethical decision making. Autonomy allows healthcare teams to respect and support a patient's decision to accept or refuse life-sustaining ...
Sep 5, 2023 · The nursing code of ethics closely resembles the American Medical Association’s Code of Medical Ethics, which covers patient-doctor relationships, consent and medical decision-making, privacy, genetics, end-of-life care, and many other issues. A burgeoning area of ethical concern is bioethics, which attempts to promote knowledge and awareness ...
Nov 29, 2023 · The American Nurses Association (ANA) has established a Code of Ethics for Nurses, which serves as a valuable resource for guiding ethical decision-making in nursing practice. The Nurse’s Code of Ethics outlines the principles and standards that nurses should uphold, ensuring professionalism, integrity, and patient-centered care.